Observation on therapeutic efficacy of thunder-fire moxibustion for hypomenorrhea after induced abortion
Lu Ying (鲁颖), Zhang Xiao-lei (张晓蕾), Gu Hai-yan (谷海燕)
1 Fengrun District Hospital of Traditional Chinese Medicine, Tangshan, Hebei Province, Tangshan 063000, China
2 Tangshan Hospital of Traditional Chinese Medicine, Hebei Province, Tangshan 063000, China
Abstract
Keywords: Moxibustion Therapy; Moxa Stick Moxibustion; Thunder-fire Moxibustion; Hormones; Abortion, Induced; Menstruation Disturbances; Postoperative Complications
The main symptoms of hypomenorrhea after induced abortion are reduced menstrual volume and shortened menstrual period, and its incidence is related to the injury of endometrial basal layer[1]. If hypomenorrhea is not treated, it will often develop into amenorrhea, and even affect fertility function, or lead to other diseases[2]. At present, Western medicine mainly uses estrogen and progesterone cycle treatment to manage this condition. Although it has a certain effect, the treatment cycle is long, and it is easy to relapse after the withdrawal.
Hypomenorrhea falls into the category of irregular menstruation. Traditional Chinese medicine (TCM) believes that the pathogenesis of hypomenorrhea after induced abortion should be deficiency of both qi and blood, and blood stasis in the uterus[3]. Abortion consumes qi and blood, causing deficiency of qi and blood. Qi deficiency fails to promote blood circulation, and then the blood stasis accumulates in the uterus. If the blood stasis is not removed, new blood will not be produced, thus resulting in hypomenorrhea.
Thunder-fire moxibustion has effects of invigorating qi and blood, promoting blood circulation for removing obstruction in collaterals. In this study, we observed the effect of thunder-fire moxibustion on hypomenorrhea after induced abortion, and compared it with sequential hormone therapy.
1 Clinical Materials
1.1 Diagnostic criteria and criteria for syndrome differentiation
This study referred the diagnostic criteria of hypomenorrhea in theGynecology of Traditional Chinese Medicine[4]: the menstrual cycle is basically normal, with menstrual volume less than 30 mL or menstrual period less than 2 d lasting for more than two successive menstrual cycles.
According to theGuiding Principles for Clinical Study of New Chinese Medicines[5], the criteria for syndrome differentiation of deficiency of both qi and blood and static blood blocking collaterals were established. Primary symptoms: little menstrual volume, purplish menstrual blood with clots, fatigue, and sallow complexion. Secondary symptoms: panting and laziness to speak, palpitations, insomnia, thirst without desire to drink, soreness and pain of the low back and knees, dark red tongue with purple spots, deep thready pulse. It could be diagnosed with 3 primary symptoms and 4 secondary symptoms, or with 2 primary symptoms and 6 secondary symptoms.
1.2 Inclusion criteria
Those who met the above diagnostic criteria of hypomenorrhea and criteria for TCM syndrome differentiation of deficiency of both qi and blood and static blood blocking collaterals; aged 20-35 years old; with normal menstruation before induced abortion, but suffered hypomenorrhea within 3 months after the abortion; not receiving medication or TCM treatment for this disease within 2 weeks before the enrollment; agreed to participate in this clinical trial and signed informed consent.
1.3 Exclusion criteria
Patients with hypomenorrhea caused by hypogonadism, dysplasia of the uterus, polycystic ovary syndrome, endometrial tuberculosis and premature ovarian failure; combined with thyroid dysfunction, hematopathy or gynecologic tumor; who had oral contraceptives recently; those with skin allergies or allergies to sex hormone drugs.
1.4 Elimination and dropout criteria
Those who did not complete the treatment as the protocol required, or those with incomplete data; those presenting with severe adverse reactions or dropped out during the trial; who was found out to unmeet the inclusion criteria after grouping; those lost to follow-up after treatment; those took other medications or accepted other therapies.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 20.0 statistical software. Measurement data were all in normal distribution, and expressed as mean ± standard deviation (±s), and the comparison of the data was analyzed byt-test. Counting data were expressed as rate and processed by Chi-square test.P<0.05 was considered to indicate a statistically significant difference.
1.6 General data
A total of 74 patients with hypomenorrhea after induced abortion were enrolled from Fengrun District Hospital of Traditional Chinese Medicine, Tangshan, Hebei Province, between September 2018 and December 2019. All patients were randomly divided into an observation group and a control group by simple random number table, with 37 cases in each group. During the trial, 1 case was eliminated from the observation group and 1 case dropped out, and 1 case was eliminated from the control group and 2 cases dropped out. A total of 69 patients finished the treatment, including 35 cases in the observation group and 34 cases in the control group. There were no significant differences in the general data between the two groups before treatment (allP>0.05), (Table 1).
Table 1. Comparison of general data between the two groups (±s)
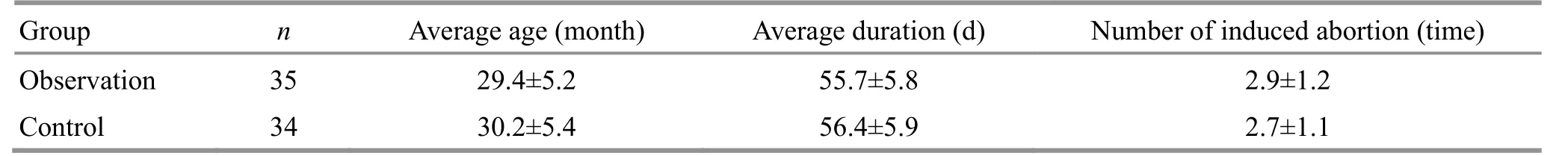
Table 1. Comparison of general data between the two groups (±s)
Number of induced abortion (time) 2.9±1.2 2.7±1.1
2 Treatment Methods
2.1 Observation group
Acupoints: Bilateral Quchi (LI 11), Zhigou (TE 6), Zusanli (ST 36) and Sanyinjiao (SP 6).
Methods:The patient took a supine position and received thunder-fire moxibustion treatment. Moxa stick especially made for thunder-fire moxibustion was selected (25 g/stick, Zhao’s Thunder-Fire Moxibustion Institute of Traditional Medicine, China). Ingredients of moxa stick:Ai Ye(Folium Artemisiae Argyi),Ru Xiang(Olibanum),Qiang Huo(Rhizoma Notopterygii),Chuan Shan Jia(Squama Manitis), artificialShe Xiang(Moschus),Mu Xiang(Radix Aucklandiae),Yin Chen(Herba Artemisiae Scopariae),Gan Jiang(Rhizoma Zingiberis),Chen Xiang(Lignum Aquilariae Resinatum) andDi Bai Zhi(Herba Selaginellae Moellendorfii). Ignited one end of the moxa stick, fixed it in the thunder-fire moxibustion box, placed it 2-3 cm away from the skin, and pointed the thunder-fire moxibustion towards the corresponding acupoint. The moxibustion treatment was performed 10-15 min for each point to appropriately make the topical skin reddish and warm-hot. The treatment was performed once a day, 5 times a week, with an interval for 2 d. And the treatment continued for 3 menstrual cycles but stopped during the menstrual period.
2.2 Control group
Patients in the control group received conventional estrogen-progesterone sequential therapy. Estradiol valerate [State Food and Drug Administration (SFDA) Approval No.: J20171038, Guangzhou Branch of Bayer Healthcare Co., Ltd., China] was taken starting from 5th day of the menstruation, 1 mg/time, once a day, for 21 d. And medroxyprogesterone acetate tablets (SFDA Approval No.: H33020715, Zhejiang Xianju Pharmaceutical Co., Ltd., China) were added orally on the 17th day of taking estradiol valerate, 10 mg/time, once a day, for 5 d. Menstruation occurred 3-7 d after withdrawal. The treatment continued for 3 menstrual cycles.
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 TCM symptom scores
According to the quantification table of TCM symptom classification in theGuiding Principles for Clinical Study of New Chinese Medicines[5], the TCM symptoms scoring table in this study was established. TCM symptoms included purplish menstrual blood with blood clots, fatigue, sallow complexion, soreness and pain of the low back and knees and insomnia. According to the degrees of none, mild, moderate and severe, the symptoms were scord 0, 2, 4 or 6 points respectively.
3.1.2 Menstrual volume
The menstrual volume of the latest cycle was calculated by the rough estimating table of menstrual volume[6]. Specific steps: recorded the number and usage of sanitary napkins (tampons) used every day. The menstrual volume was estimated according to the corresponding relationship of menstruation pictogram (blood dripping in the toilet and blood lost from blood clots should be counted). The last menstrual volume before treatment and the menstrual volume during the first 5 d of the first menstruation after treatment were estimated.
3.1.3 Endometrial thickness
Siemens color Doppler ultrasound s3000 was used to detect the endometrium thickness in transabdominal manner. The examination was performed 5 d before the last menstruation before treatment and 5 d before the first menstruation after treatment.
3.1.4 Sex hormone levels
Five milliliter fasting elbow venous blood was collected in early morning, and centrifuged at 4 000 r/min for 10 min at low temperature to separate serum. Progesterone (P), follicle-stimulating hormone (FSH), luteinizing hormone (LH) and estradiol (E2) were measured by chemiluminescence immunoassay. The hormone levels were measured 5 d before the last menstruation before treatment and 5 d before the first menstruation after treatment.
3.2 Criteria of curative efficacy
According to the criteria of curative efficacy in the
Guiding Principles for Clinical Study of New Chinese Medicines[5], combined with therapeutic effect index, the curative efficacy was assessed.
The therapeutic effect index = (TCM symptom scores before treatment - TCM symptom scores after treatment) ÷ TCM symptom scores before treatment × 100%.
Cured: The therapeutic effect index was ≥90%.
Markedly effective: The therapeutic effect index was ≥60%, but <90%.
Effective: The therapeutic effect index was ≥30%, but <60%.
Invalid: The therapeutic effect index was <30%.
3.3 Results
3.3.1 Comparison of the clinical efficacy
The total effective rate was 91.4% in the observation group and 73.5% in the control group. The difference between the two groups was statistically significant (P<0.05), (Table 2).
3.3.2 Comparison of TCM symptom scores
There were no significant differences in the TCM symptom scores between the two groups before treatment (P>0.05). After treatment, the TCM symptom scores of both groups decreased significantly (allP<0.05), and each TCM symptom score in the observation group was lower than that in the control group (allP<0.05). The above results suggested that both therapies could improve TCM symptoms in patients with hypomenorrhea after induced abortion, and thunder-fire moxibustion had a better efficacy (Table 3).
3.3.3 Comparison of endometrial thickness and menstrual volume
There were no significant differences in the endometrial thickness and menstrual volume between the two groups before treatment (bothP>0.05). After treatment, the endometrial thickness and menstrual volume in both groups increased significantly (allP<0.05), and the improvements in the observation group were superior to those in the control group (bothP<0.05). The above results suggested that both therapies could increase endometrial thickness and menstrual volume for patients with hypomenorrhea after induced abortion, but thunder-fire moxibustion had better effects (Table 4).
3.3.4 Comparison of serum P, FSH, LH and E2levels
There were no significant differences in the serum levels of P, FSH, LH and E2between the two groups before treatment (allP>0.05). After treatment, the serum levels of P, FSH, LH and E2increased in both groups (allP<0.05), and the improvements in the observation group were more notable than those in the control group (allP<0.05). The above results suggested that both therapies could improve the serum levels of P, FSH, LH and E2for patients with hypomenorrhea after induced abortion, but thunder-fire moxibustion had better effects (Table 5).
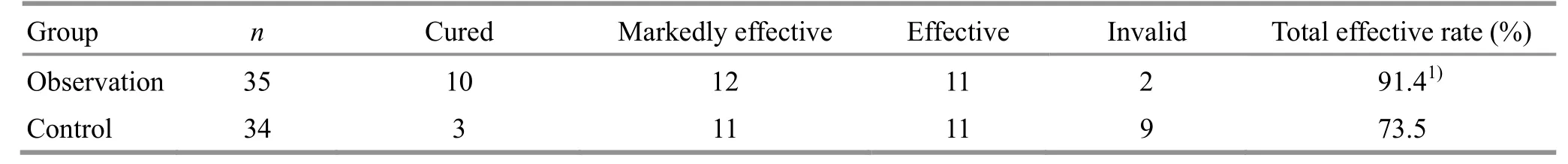
Table 2. Comparison of clinical efficacy between the two groups (case)
Table 3. Comparison of TCM symptom scores between the two groups (±s, point)
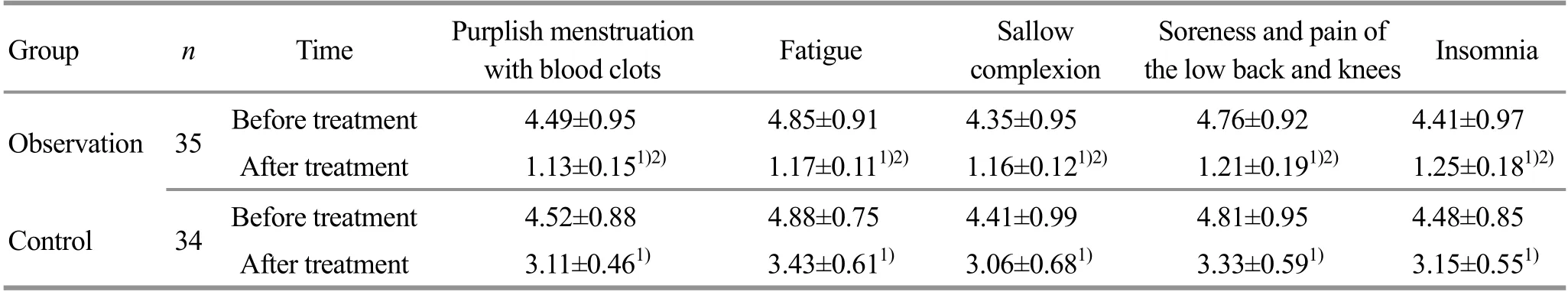
Table 3. Comparison of TCM symptom scores between the two groups (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time Purplish menstruation with blood clots Fatigue Sallow complexion Soreness and pain of the low back and knees Insomnia Observation 35 Before treatment 4.49±0.95 4.85±0.91 4.35±0.95 4.76±0.92 4.41±0.97 After treatment 1.13±0.151)2) 1.17±0.111)2) 1.16±0.121)2) 1.21±0.191)2) 1.25±0.181)2) Control 34 Before treatment 4.52±0.88 4.88±0.75 4.41±0.99 4.81±0.95 4.48±0.85 After treatment 3.11±0.461) 3.43±0.611) 3.06±0.681) 3.33±0.591) 3.15±0.551)
Table 4. Comparison of endometrial thickness and menstrual volume between the two groups ( ±s)
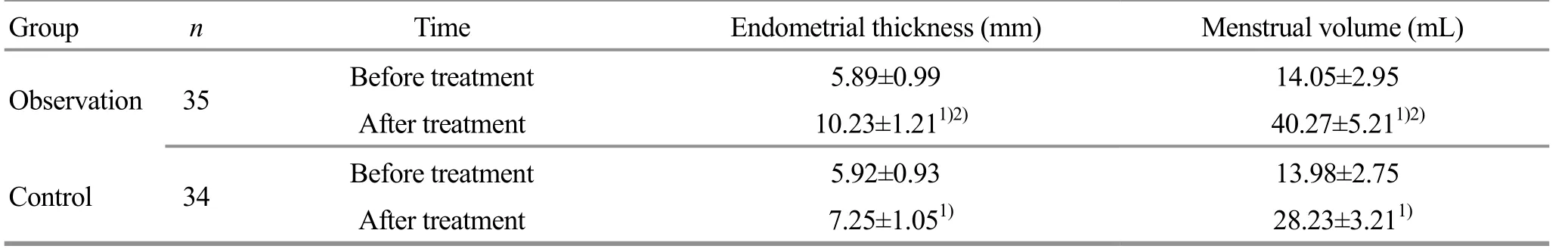
Table 4. Comparison of endometrial thickness and menstrual volume between the two groups ( ±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Menstrual volume (mL) 14.05±2.95 40.27±5.211)2) 13.98±2.75 28.23±3.211)
Table 5. Comparison of serum P, FSH, LH and E2 levels between the two groups (±s)

Table 5. Comparison of serum P, FSH, LH and E2 levels between the two groups (±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time P (μg/L) FSH (IU/L) LH (IU/L) E2 (ng/L) Observation 35 Before treatment 0.76±0.16 4.34±0.82 3.51±0.76 35.58±5.12 After treatment 7.31±2.351)2) 8.13±2.191)2) 5.99±1.011)2) 48.37±7.191)2) Control 34 Before treatment 0.72±0.14 4.11±0.77 3.49±0.66 36.08±6.11 After treatment 4.13±1.591) 6.57±1.951) 4.45±0.901) 42.15±6.901)
4 Discussion
Hypomenorrhea is a common complication after induced abortion, related to excessive suction and curettage during the surgery, injury to the endometrial basal layer, and scar formation[7]. Meanwhile, the decrease in blood supply to the endometrium caused by thin endometrium and intrauterine adhesions are also causes of hypomenorrhea[8]. Hypomenorrhea can cause endometriosis, cervicitis, menstrual arthritis, menstrual skin rash, menstrual toothache, menstrual asthma and acne[9]. In severe cases, it may lead to reproductive dysfunction.
At present, treatment of Western medicine for hypomenorrhea after induced abortion mainly is estrogen-progesterone sequential therapy, which can increase the menstrual volume and endometrial thickness, meanwhile regulating the sex hormone levels[10]. However, long-term application may cause adverse reactions, even disorder of gonadal axis[11].
TCM believes that hypomenorrhea after induced abortion is caused by the injury of qi and blood after surgery, and blood stasis blocking the uterus[12]. The treatments should be based on tonifying qi and blood, and removing blood stasis for unblocking collaterals.
In this study, Quchi (LI 11), Zhigou (TE 6), Zusanli (ST 36) and Sanyinjiao (SP 6) were selected for thunder-fire moxibustion. Women take blood as the foundation, and take qi as the commander, so that the menstruation occurs on time. Quchi (LI 11) is the He-Sea point of the Large Intestine Meridian which has plenty of qi and blood. Quchi (LI 11) has effects of harmonizing qi and blood, relieving meridians and unblocking collaterals, and can be applied in the treatment of menopathy[13]. Zusanli (ST 36) is the He-Sea point of the Stomach Meridian, with effects of tonifying qi and blood[14]. Modern research suggests that thunder-fire moxibustion at Zusanli (ST 36) can improve the clinical symptoms of hypomenorrhea and increase menstrual volume[15]. Zhigou (TE 6) can regulate and smooth qi movement in three Jiao (triple energizer), so that the tonified qi-blood can normally circulate, avoiding the blockage of qi movement[16]. Modern research suggests that Zhigou (TE 6) can treat gynecologic and reproductive diseases, with little adverse reaction[17]. Sanyinjiao (SP 6) is the crossing point of the Spleen Meridian, Liver Meridian and Kidney Meridian, with effects of invigorating spleen and benefiting qi, regulating and tonifying liver and kidney[18]. Modern research suggests that stimulating Sanyinjiao (SP 6) can significantly improve the sex hormone levels in patients with hypomenorrhea, and increase the endometrial thickness and menstrual volume[19]. The combination of the above four acupoints can achieve the effects of tonifying qi and blood, activating blood and unblocking collaterals.
Zhao’s thunder-fire moxibustion has been improved on the basis of thunder-fire miracle needle. The main medicinal materials includeAi Ye,Ru Xiang,Qiang Huo,
Chuan Shan Jia, artificialShe Xiang,Mu Xiang,Yin Chen,Gan Jiang,Chen XiangandDi Bai Zhi. The combination of the above ingredients has effects of warming meridians for dispelling cold, and benefiting qi for unblocking collaterals[20]. Thunder-fire moxibustion, as an external therapy, treats diseases through the warm-heat of moxibustion and the topical stimulation of medicinal materials. Also, it can achieve the whole regulation through absorption and metabolism of medicinal materials, transmission of meridians and neuroregulation[21].
The menstrual volume, endometrial thickness and sex hormone level can reflect the macro and micro situation of patients with hypomenorrhea, and can be used for disease diagnosis and prognosis estimation. TCM syndrome can fully reflect the overall situation of patients with hypomenorrhea. Results in this study suggested that: after treatment of 3 menstrual cycles, the total effective rate in the observation group was significantly higher than that in the control group (P<0.05), and the TCM symptom scores of the observation group were significantly lower than those of the control group (P<0.05); the improvements in menstrual volume, endometrial thickness and serum sex hormone levels in the observation group were also superior to those in the control group (allP<0.05). These showed that thunder-fire moxibustion was effective in treating hypomenorrhea after induced abortion, and was better than hormone sequential therapy.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by 2019 Traditional Chinese Medicine Scientific Plan Project of Hebei Provincial Administration of Traditional Chinese Medicine (2019年 度河北省中医药年理局中医药类科研计划课题, No. 2019231).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 20 January 2020/Accepted: 3 April 2020
 Journal of Acupuncture and Tuina Science2021年1期
Journal of Acupuncture and Tuina Science2021年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Effect of electroacupuncture on calcium-activated chloride channel currents in interstitial cells of Cajal in rats with diabetic gastroparesis
- Effect of electroacupuncture pretreatment on the protein expression of c-fos in fastigial nucleus and lateral hypothalamus area in rats with acute myocardial ischemia-reperfusion injury
- Effect of herb-partitioned moxibustion in improving tight junctions of intestinal epithelium in Crohn disease mediated by TNF-α-NF-κB-MLCK pathway
- Ginger-partitioned moxibustion plus pediatric massage for treating infantile diarrhea due to spleen deficiency: a randomized controlled clinical trial
- Efficacy observation of long-retaining scalp acupuncture plus interactive training for upper-extremity dysfunction after cerebral stroke
- Clinical observation on the time-effect relationship of moxibustion for primary dysmenorrhea due to stagnation and congelation of cold-damp
