COVID-19流行期间体力活动助力疫情防控的潜在生物学机制
韩娜娜 王爱文 余蕾 李阳 黄晖明
摘 要:2019年新型冠状病毒肺炎(COVID-19)的疫情暴发和流行,在健康、经济和生活方式方面对人类社会造成了前所未有的威胁,持续社交隔离导致的体力活动不足会降低人体抵御病毒感染的能力,对免疫、呼吸、心血管、肌肉骨骼系统以及心理产生损害。体力活动对COVID-19疫情是否具有主动防控的潜在作用,其内在机制如何?基于既往研究和COVID-19最新相关数据,从COVID-19及其病原体新型冠状病毒(SARS-CoV-2)密切关联的生物学角度[ACE2-Ang(1-7)-Mas轴、免疫系统、心理、心肺功能方面],综述了体力活动对COVID-19防控潜在的生物学机制。综合显示:COVID-19病原体(SARS-CoV-2)可通过ACE2感染多个脏器细胞,主要与ACE2-Ang(1-7)-Mas轴的下调、ACE-Ang II-AT1R通路的过度激活有关,而体力活动可以激活ACE2-Ang(1-7)-Mas轴,调节两者之间的平衡;适当的体力活动对增强免疫功能和降低病毒感染的风险、持续时间和严重性有益;体力活动还可通过调节人体交感神经系统等降低人的焦虑和抑郁水平;适当的体力活动可提高心肺适能、减轻全身炎症反应,降低斑块破裂风险。
关键词:体力活动;新冠肺炎;ACE2;免疫系统;生物学机制
中图分类号:G 804.55 学科代码:040302 文献标识码:A
Abstract:The outbreak and epidemic of novel coronavirus pneumonia(COVID-19) has caused hitherto unknown threat to human society in health, economy and lifestyle. Continuous physical activity caused by social distancing can reduce the risk of human body against virus infection, and damage the immune system, respiratory system, cardiovascular system, musculoskeletal system and psychology. Does physical activity have the potential function of active prevention and control of COVID-19 pandemic, and what is its internal mechanism? Novel coronavirus (SARS-CoV-2) is closely related to COVID-19 and its pathogen [ACE2-Ang (1-7) - Mas axis, immune system, psychology, cardiopulmonary function] based on previous research and the latest evidence of COVID-19. The potential biological mechanism of physical activity on COVID-19 prevention and control is reviewed. The results show that COVID-19 pathogen (SARS-CoV-2) could infect multiple organ cells through ACE2, which was mainly related to the down regulation of ACE2-Ang (1-7) - MAS axis and the over activation of CE-Ang II-AT1R pathway, while physical activity could activate ACE2- Ang (1-7) - MAS axis and regulate the balance between them; appropriate physical activity is beneficial to enhance immune function and reduce the risk, duration and severity of virus infection; physical activity can also reduce peoples anxiety and depression by regulating human sympathetic nervous system; appropriate physical activity can improve cardiopulmonary fitness, reduce systemic inflammatory response and reduce the risk of plaque rupture.
Keywords:physical activity; COVID-19; ACE2; immune system; biological mechanism
隨着COVID-19大流行的持续,各个国家或地区积极采取社交隔离措施,防止人与人之间的传播[1]。由于针对COVID-19的最终疫苗、特效药物和治疗方法短期尚不能确定[2]。密切接触者追踪和社交隔离是目前控制COVID-19疫情最有效的手段[3]。全国范围内的大规模隔离,已在中国被证明有效地遏制了COVID-19疫情,同时也限制了境外感染病例的输入[4-5]。COVID-19大流行是一场前所未有的人类健康危机,居家几个星期到几个月的自我隔离,对个体同时也是一项具有重大健康风险的生理挑战。持续的社交隔离导致的体力活动不足会降低机体抵御病毒感染的能力,对免疫、呼吸、心血管、肌肉骨骼系统以及心理产生损伤,可能对全社会形成“第二次”健康威胁[6-7]。各国政府也积极探索和采取主动性疫情应对策略,为应对COVID-19大流行,WHO、多国疾病预防与控制中心及其他公共卫生咨询组织鼓励个人在不违反法律规定和遵守公共卫生和社区安全管理规定的情况下开始或继续参与体力活动,以保持身心健康[8]。
目前,我国已经有序复工、复产、复课,但全球COVID-19疫情仍然很严峻,部分疫情严重的国家仍然处于社交隔离状态。由于疫情的不确定性,我国疫情面临着波动和反复的暴发风险,未来居家隔离或社交隔离的防控措施可能重复使用。体力活动包括交通出行、工作、家务中的身体活动以及闲暇运动锻炼,是体医融合的重要组成部分[9]。当前,我国已进入疫情常态化防控时期,体力活动对COVID-19是否具有主动防控的潛在作用?其内在机制如何?这将影响到公共机构疫情防控的应对政策、措施,也将影响个体的健康认知和主动防控策略。本文基于既往研究和COVID-19最新相关数据,从COVID-19及其病原体新型冠状病毒(SARS-CoV-2)密切关联的生物学角度[ACE2-Ang(1-7)-Mas轴、免疫系统、心理、心肺功能方面],综述了体力活动对COVID-19防控潜在的生物学机制,为体力活动有利于COVID-19疫情防控提供理论依据,并提供相关的体力活动应对策略与建议。
1 COVID-19与ACE2-Ang(1-7)-Mas轴、免疫系统、心理、心肺功能的关联性
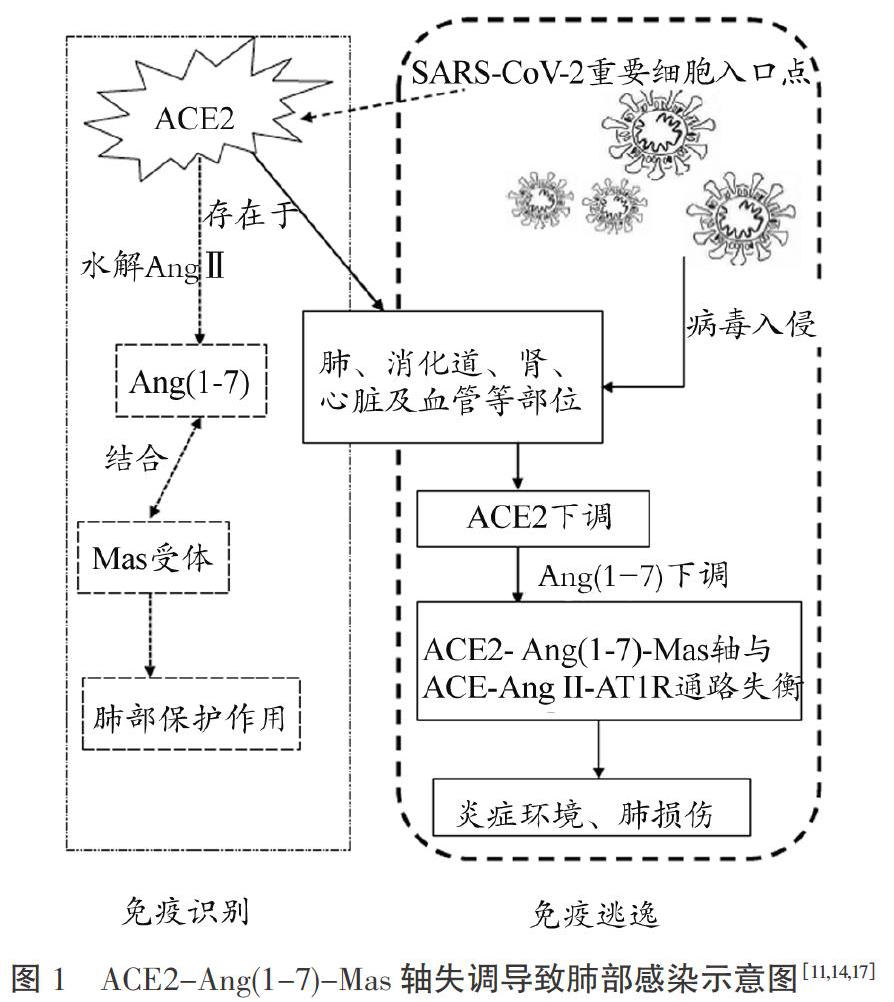
血管紧张素转换酶2(ACE2)是一种I型跨膜蛋白,是人体组织中肾素-血管紧张素系统(RAS)的主要调节剂,可调节血管收缩。ACE2可将血管紧张素Ⅱ(AngⅡ) 水解为Ang (1-7),Ang(1-7)的主要受体为Mas受体(MasR),共同构成ACE2- Ang(1-7) -Mas轴,起到拮抗ACE-Ang II-血管紧张素1型受体(AT1R)通路的作用[10]。ACE2-Ang(1-7)-Mas轴和ACE-Ang II-AT1R通路被视为两个相反但互补的通路。ACE2-Ang(1-7)-Mas轴具有利钠利尿、调节水电解质平衡,抗炎和抗纤维化作用[11]。多项研究显示,ACE2与SARS-CoV-2相关,且被认为是SARS-CoV- 2的重要细胞入口点[12-13]。从致病机制上说,病原体SARS-CoV-2可通过ACE2感染多个脏器细胞,引发一系列免疫反应,正常免疫状态下,机体能杀死病毒。若免疫延迟或过强,则可引起机体的反应,SARS-CoV-2与ACE2结合消耗了ACE2,进而下调了ACE2- Ang( 1-7) -Mas轴,使ACE2-Ang(1-7)-Mas轴和ACE-Ang II-AT1R通路的调节失衡,过度激活了ACE-Ang II-AT1R通路[14]。由于较少的ACE2可将血管紧张素转化为Ang( 1-7 ),并产生抗炎和抗纤维化通路,导致炎症环境和肺损伤,肺部毛细血管通透性增加,出现急性肺衰竭[15-16],原理如图1所示。
流感病毒和冠状病毒可导致发病率和死亡率,特别是免疫功能低下的易感人群。免疫力的下降会增加机体各器官对病原体的易感性,最终导致机体各器官和人体系统的一系列病变。本次COVID-19是由SARS-CoV-2引起的呼吸道传染病[18],与其他冠状病毒一样,SARS-CoV-2的人际传播主要是呼吸道飞沫传播感染[19]。COVID-19流行期间人体先天免疫力的下降会致使流感病毒和冠状病毒更容易和更快速地入侵人体,引发呼吸道感染。此外,研究表明与重症COVID-19患者相比,轻症患者淋巴细胞的减少和心血管疾病的发生率均较低,淋巴细胞可能在这其中产生重要作用[20-23]。淋巴细胞的减少意味着人体免疫力下降、易于被病毒入侵,其中自然杀伤(NK)细胞又被认为是机体最重要的免疫细胞之一。它通过对病毒、肿瘤、炎症等靶标进行作用,从而使机体具有抗病毒、抗炎等功能,起到防治冠状病毒感染的重要作用[24]。目前,由于要获得安全有效的疫苗需要一段时间,当务之急是利用提高先天免疫来加速早期抗病毒免疫反应[25]。
根据灾难心理健康理论[26]和风险认知理论[27],突发公共卫生事件会引发一些人产生更多负面的情绪和认知评估等。我国的一项研究报告显示,接触过COVID-19信息的卫生保健工作者中,抑郁、焦虑、失眠和痛苦这些情绪的比例很高,尤其是直接参与COVID-19患者诊断、治疗和护理的医护人员[28],由于COVID-19的不确定性,加之身体和心理的疲惫,易产生心理健康问题[29]。而对于大众来说,居家隔离被认为是降低感染率和避免卫生系统超负荷工作的有效方法,并且在我国已经得到有效印证,但长时间的社交隔离或居家封闭会使一些人产生压力和情绪问题。COVID-19疫情防控隔离期间,人们消极情绪的主要来源是感染恐惧、沮丧、无聊、供应不足、信息不足、经济损失等,这些消极情绪最终会发展为焦虑和抑郁。Li 等调查了COVID-19疫情信息通报对微博用户情绪的影响,结果发现大众的消极情绪(例如:焦虑、抑郁和愤怒)以及对社会风险的敏感性增加,而积极情绪(例如幸福感)和对生活的满意度下降;疫情期间人们更关心的是自己和家庭成员的健康状况,而不是朋友也不是休闲娱乐[30]。对COVID-19暴发期间澳大利亚成年人的心理健康调查结果显示,在一种或多种心理困扰状态中,女性及未恋爱、收入最低的女性、18~45岁或患有慢性疾病的女性心理负变化的得分明显较高。分析其原因得出:身体活动、睡眠、吸烟和酒精摄入的消极变化与较高的抑郁、焦虑和压力症状有关[31]。此外,最新研究对我国COVID-19大流行期间普通人群心理健康的调查结果显示,27.9%的参与者有抑郁症状,31.6%有焦虑症状,29.2%有失眠症状,24.4%的参与者有急性应激症状。而与消极心理健康结果相关的因素包括:确诊或疑似COVID-19,有确诊或疑似COVID-19的亲属,有职业接触风险,生活在湖北省,并经历隔离和延迟返回工作[32]。因此,无论是在疫情暴发期还是随后的疫情常态化防控期,及时了解COVID-19可能引起的心理变化并采取有效措施至关重要。
COVID-19暴发以来,长时间的居家隔离使人们体力活动不足、久坐时间增加、营养过剩,从而导致心肺功能下降以及慢性疾病风险增加[33-34]。仅仅几天的久坐生活方式就足以导致肌肉损失、神经肌肉接头损伤和纤维失神经、胰岛素抵抗、有氧能力下降、脂肪沉积和低度全身炎症[34]。在一般人群中,缺乏体力活动与低度全身炎症以及随后的心肺功能下降、心血管疾病风险增加有关[35]。同时,已知COVID-19重症患者会出现呼吸困难甚至呼吸窘迫等临床症状,最新调查结果显示超过 30%的患者需要使用呼吸机,不良后果是可能导致膈肌萎缩、收缩功能障碍和呼吸肌无力,肺功能受损[36]。与此同时,由于长时间的社交隔离导致久坐行为增加、体力活动水平大幅度下降,人的心肺功能和其他身体素质受到损害[33]。
综上所述,COVID-19及其病原体SARS-CoV- 2与ACE2-Ang(1-7)-Mas轴、免疫系统、心理、心肺功能4个生物学角度具有密切的关联性。SARS-CoV-2可通过ACE2感染多个脏器细胞,使ACE2-Ang(1-7)-Mas轴和ACE-Ang II-AT1R通路的调节失衡,引发一系列免疫反应;COVID-19流行期间,长时间的社交隔离以及缺乏体力活动导致肌肉萎缩和虚弱、肥胖、血生化异常、心肺功能下降,对免疫系统、情绪造成不良影响。
2 体力活动有助于COVID-19疫情防控的潜在作用机制
基于既往的研究,我们知道体力活动对ACE2-Ang(1-7)-Mas轴调节、免疫调节、情绪调控、心肺功能提升发挥着积极作用。那么,体力活动是否通过这些机制对COVID-19疫情产生主动防控的作用?阐述体力活动潜在生物学机制,在COVID-19疫情防控常态化期间,有助于为公众重返积极体力活动提供理论依据。
2.1 体力活动调节ACE2-Ang(1-7)-Mas轴
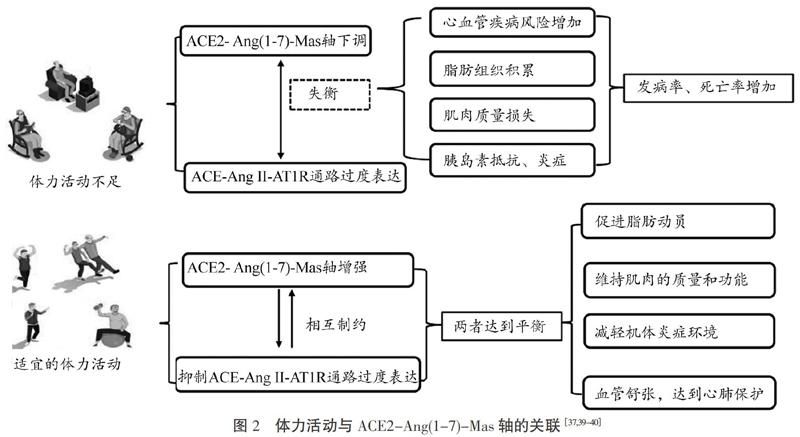
维持或恢复ACE2-Ang(1-7)-Mas轴和ACE-Ang II-AT1R通路之间的自然平衡,可作为一种减轻COVID-19的易感性和严重性可能的手段。Nunessilva 等研究表明适当体力活动可以增强ACE2-Ang(1-7)-Mas轴,同时抑制ACE-Ang II-AT1R通路[37]。Peng 等通过动物实验测试了高血压前期适当的运动训练是否能预防自发性高血压大鼠(SHR)的高血压和心脏重构,并通过检查心脏血管紧张素转换酶(ACE)和ACE2信号传导轴来探索其潜在机制,结果发现高血压前期进行运动训练可以减轻高血压和心脏重塑,而在运动期间Ang II的下调是一种保护机制[38]。有研究对慢性心力衰竭的家兔进行了运动训练干预,结果发现慢性心力衰竭家兔脑组织中的ACE和ACE2恢复正常。运动训练可以使慢性心力衰竭家兔的中枢神经系统中的ACE降低并增加ACE2的表达,从而使ACE和ACE2之间恢复平衡[39]。此外,在白色脂肪中,ACE-Ang II-AT1R通路的上调可促进脂肪生成,并减少脂肪分解和脂肪生成,导致脂肪细胞肥大和脂质存储,从而增加了胰岛素抵抗和炎症。在骨骼肌中,ACE-Ang II-AT1R通路促进蛋白质降解并增加炎症状态和氧化应激,导致肌肉消瘦。但ACE2-Ang(1-7)-Mas轴可通过抵抗Ang II的作用起反调节作用,有研究表明,运动训练可将RAS的平衡移向ACE2-Ang(1-7)-Mas轴,在刺激ACE2-Ang(1-7)-Mas轴的同时促进了ACE-Ang II-AT1R通路的抑制,从而促进了脂肪的动员以及肌肉质量和功能的维持[40](见图2)。虽然COVID-19是否会造成长期的心肺损伤还有待研究。但如果患者愈后确实需要心肺康复,运动可能是首选的治疗方法,运动训练可以激活ACE2-Ang(1-7)-Mas轴,减少肺纤维化[41]。
2.2 體力活动影响免疫力与传染病感染风险
多项研究表明,无论是2009年的甲型H1N1流感病毒[42-43],还是2019年的COVID-19,年龄大、肥胖和有慢性基础疾病的人群最容易感染传染病,且愈后身体状况相对较差,对重症监护资源的需求更高[21]。随年龄的增长,免疫系统衰老也被认为是老年人对疫苗的反应效果差、患传染病和恶性肿瘤概率高的主要原因,但运动可能有助于恢复衰老的免疫系统[44]。Kostka 等的研究表明,年龄在66~84岁之间、经常维持适当体力活动的老年人,其被感染上呼吸道感染的概率和感染天数均较低[45]。同时,体力活动与感染之间存在剂量-反应关系,高水平体力活动的成年人被感染的风险最低,低水平体力活动的成年人被感染的风险最高[46]。此外,有规律的运动被证明可以提高人体对疫苗的反应[47]。Simpson 等研究表明,定期的运动与疫苗接种反应增强、疲惫/衰老的T细胞数量减少、炎性细胞因子的循环水平降低、中性粒细胞吞噬活性增加以及炎症反应降低有关[48]。目前还没有针对COVID-19的有效药物[49],人们通过营养和锻炼等非药物的方式提高免疫力。而体力活动也早已被证实可以显著降低人体发生全身炎症、损伤免疫功能的非传染性慢性疾病的风险[50]。运动免疫领域研究的普遍共识是,免疫系统对运动的反应取决于运动的强度、持续时间和运动类型[51-52]。
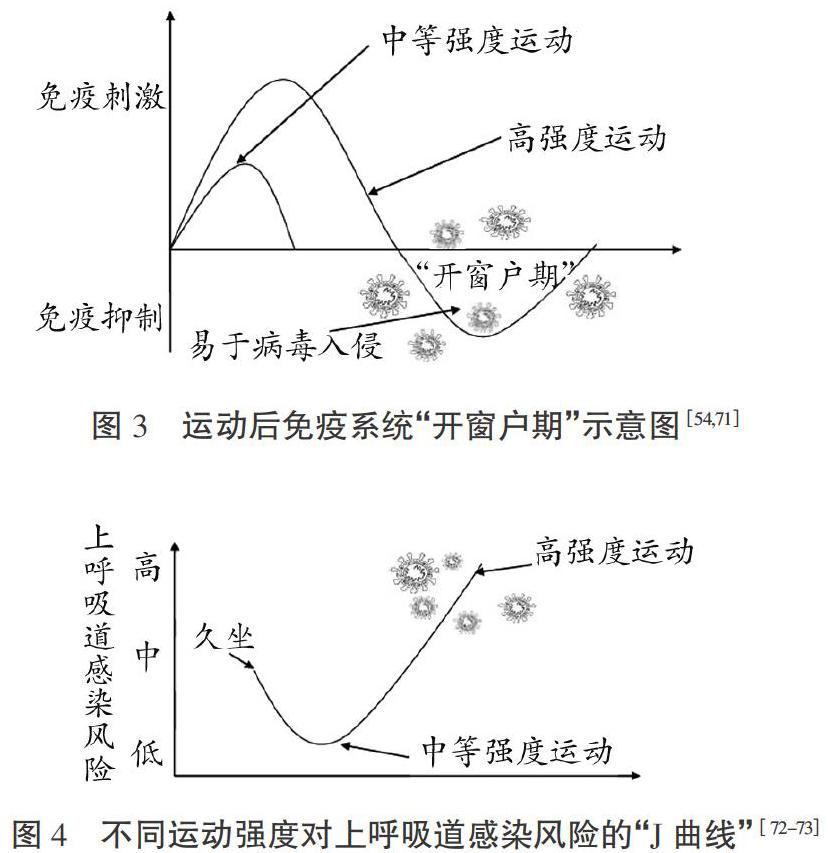
免疫系统对运动的反应取决于运动的强度,不同强度的体力活动对免疫系统的影响不同[51] 。体力活动可以通过增加免疫细胞来改善免疫健康,适量的运动可以改变人体血液中NK 细胞的百分比[53]。免疫力的增强可能是由于经常锻炼的人NK 细胞的数量发生改变或功能得到了增强[24,54]。有研究表明,高强度运动对肥胖患者的炎症因子有积极影响[55-56]。但值得注意的是,休息不充分的情况下进行长时间的间歇或高强度训练,会导致免疫抑制和增加人体对感染性疾病的易感性[57]。长时间高强度运动也会导致炎症介质水平升高,可能会增加受伤和慢性炎症的风险,而中等强度或休息充分情况下的高强度运动可以达到最大的益处[58]。Warren 等的小鼠实验新证据表明,在感染前进行中等强度的运动可以改善对感染性病原体的免疫应答,从而将感染的严重程度降到最低[59]。有关流感的研究表明,经常进行低、中等强度运动的患者比从不或很少运动的患者的死亡率明显低(优势比为0.62)[60]。还有多项研究表明,规律性中高强度体力活动者上呼吸道感染的发病率比低强度者低[61-63]。同时,越来越多的实验和动物模型研究也阐明了中等强度体力活动对病毒性呼吸道感染的潜在预防作用[64-67]。Davis 等的小鼠研究表明,适当的体力活动可降低呼吸道感染的易感性,改善抗病毒淋巴细胞功能[68]。免疫系统“开窗户期”理论(见图3)可以解释高强度运动的风险,其特征是高强度运动后免疫系统受到抑制,同时增加上呼吸道疾病的易感性[69]。由图4可见,不同运动强度与上呼吸道感染的风险呈现J形曲线,“J曲线”表明经常进行中等强度运动锻炼可以提高人的免疫力,过度的长时间运动训练会损伤机体的免疫功能[44]。随着COVID-19疫情在中国逐步好转,并加强了核酸检测力度,更多无症状感染者被发现,这些患者均无任何临床症状[70]。剧烈的高强度运动对无症状感染者可能更危险,一旦免疫受到抑制就可能出现COVID-19症状,并且增加了传播风险。因此,进行或维持规律的中、低强度运动是无症状感染者进行体力活动的首选方式。
免疫系统对运动的反应与运动类型有关。研究表明,太极拳和气功练习能夠改善老年人对流感疫苗的抗体反应[74]。而瑜伽可以下调促炎症因子TNF-a、IL-1、IL-6等,可作为患有炎性疾病或高炎症风险人群的补充干预措施[75]。此外,耐力运动可促进隔膜肌肉的大量生化改变,从而产生一种表型,可保护其免受破坏[76]。有研究表明,只需连续10 d的耐力训练,就能显著预防呼吸机引起的膈肌功能障碍[77-78]。Figueiredo 等的随机对照实验表明吸气肌肉训练和有氧训练改善了血液透析患者的呼吸和功能参数并调节了炎症标志物[79]。
免疫系统对运动的反应与运动持续时间有关。Lowder 等研究发现,适度的耐力锻炼(30 min/d)可以保护小鼠免于因流感死亡;在流行性感冒感染后的最初几天进行适度的耐力锻炼(30 min/d),可显著降低小鼠的死亡率。长时间运动(2.5 h/d)会导致发病率增加,并倾向于降低生存率[80]。该研究充分地证明了适当的体力活动在增强免疫功能和降低病毒感染风险上的效果。因此,一旦完全康复,轻度感染的患者可逐渐恢复体力活动和运动,如果在恢复运动过程中出现诸如心、胸痛,或呼吸困难等与运动有关的症状,则可能需要进行心脏影像学检查以排除COVID-19心脏损伤,然后再进行更高强度的体力活动。
上述间接证据均表明,日常的体力活动是优化免疫系统功能的完整性以及阻止或减弱病毒感染严重程度的一个重要策略,尤其是在免疫力低下的易感人群中。在COVID-19疫情中不建议进行长时间高强度运动,尤其是突然增加的剧烈有氧或阻力运动,运动健身应该降低任何对免疫系统产生负面影响的可能性。中等强度的体力活动作为一种非药物、廉价、简易的方式来应对COVID-19大流行是值得推荐的,做家务等日常生活中进行中等强度(每周约150 min)的体力活动对于获得最佳的免疫支持是必要的。
2.3 体力活动调控心理及情绪
体力活动可以明显降低人的焦虑和抑郁水平[81],心理神经免疫学观点认为,长期的消极情绪会降低人的免疫功能,破坏人正常生理机制的平衡[82]。体力活动通过调节人体交感神经系统、下丘脑-垂体-肾上腺轴、脑源性神经营养因子及自我效能感等机制缓解焦虑和调节情绪[83-84]。Aylett 等回顾了15项研究发现,确诊焦虑症的患者与不运动的对照患者相比,有氧运动可以有效治疗焦虑症,并且高强度比低强度运动更有效[85-86]。另有研究表明,运动后血液中血清素发生变化,这被认为在一定程度上介导了运动和抑郁之间的关系[87]。因此,即使在限制空间情况下,人们仍然应该保持体力活动。如果无法进行户外运动,在室内进行体育锻炼也可以促进人的精神健康[88],这也是目前短期内缓解负面情绪最简单而有效的方法。
2.4 体力活动提高心肺功能
体力活动过程中骨骼肌收缩产生的抗炎因子可减轻全身炎症反应,降低斑块破裂风险,从而减少心脏骤停和运动性猝死[89-90]。另外,心脏和外周肌肉被流感和冠状病毒感染时,会引发心脏组织损伤和心肌感染,进而有可能导致急性心肌梗死、心力衰竭或心律失常[91-93]。有规律的体力活动可以减少与心血管相关的一些危险因素,可使内皮功能增强,冠状动脉结构发生适应性变化、血管阻力和血压降低[94-96]。
因此,有规律的运动或有体力活动参与的生活方式对改善心肺功能、预防心血管疾病至关重要[97]。多项循证医学研究证明了心肺功能的增强与全因和心血管疾病死亡率降低之间存在关联[98-99]。这种联系存在剂量反应关系,Kodama 等通过对33个研究进行分析得出心肺功能每增加1梅脱相当于分别降低13%、15%的全因死亡和心血管死亡风险[100]。一项跟踪研究发现,校正了吸烟、健康状况和肥胖因素后,老年人(≥60岁)的心肺功能越低,其死亡率越高,心肺功能是老年人死亡率的显著预测指标[101]。COVID-19暴发以来,老年患者死亡风险最高,基础疾病和衰老的心血管生理功能使老年人特别容易受到病毒侵害。体力活动提高心肺功能水平有助于老年人抵抗病毒的感染以及降低心血管靶器官的损伤。在COVID-19大流行期间,对于普通人来说,积极的体力活动和运动锻炼会使机体维持较好的CRF、减少心血管疾病风险,但对于COVID-19患者来说,SARS-CoV-2感染期间肌细胞和冠状动脉的炎症反应会使患者处于心源性猝死的危险之中,新冠肺炎患者尸检的报告也显示如此[92-93]。因此,不建议在任何全身性病毒性疾病期间进行体力活动,体力活动可在身体完全恢复后逐渐开展。
综上所述,体力活动对COVID-19疫情发挥防控作用的潜在生物学机制主要体现在以下方面:①COVID-19的病原体SARS-CoV-2可通过ACE2感染多个脏器细胞,主要与ACE2- Ang(1-7)-Mas轴的下调、ACE-Ang II-AT1R通路的过度激活有关,而体力活动可以激活ACE2-Ang(1-7)-Mas轴,调节两者之间的平衡,从而减少肺纤维化等靶器官损伤;②适当的体力活动对增强免疫功能和降低病毒感染的风险、持续时间和严重性有益,但免疫系统对运动的反应取决于运动的强度、持续时间和类型,日常参与中等强度(每周约150 min)的体力活动可获得最佳的免疫支持;③体力活动可通过调节人体交感神经系统、下丘脑-垂体-肾上腺轴、脑源性神经营养因子等降低人的焦虑和抑郁水平,缓解不良应激下的负面心理情绪,促进人的精神健康;④适当的体力活动可提高心肺适能、减轻全身炎症反应,降低斑块破裂风险,对心血管疾病和其他慢性病具有潜在防治功效,同时对COVID-19感染者来说,具有较好的心肺功能也可以降低并发症的风险。ACE2-Ang(1-7)-Mas轴、情绪、心肺功能的良性改变与机体免疫力的提高有关,适当的体力活动可通过调节人的ACE2-Ang(1-7)-Mas轴、免疫力、心理情绪、心肺功能而有助于疫情防控。
3 COVID-19疫情防控社交隔离期体力活动建议
鉴于先前的大量证据表明,体力活动在疾病预防、慢性病辅助治疗和心理健康促进方面具有有益的作用。在COVID-19流行期间,对于相对健康的人群,维持体力活动水平是解决久坐行为、减少感染风险和减轻隔离导致的不良心理影响的关键;对于无症状感染者,维持中低强度的体力活动是有必要的,目的是使免疫力恢复到感染前的健康状态和维持体适能;对于COVID-19临床患者,不建议病毒感染期间进行体力活动。居家隔离期间,一些知名的健康或体育机构调整了国际体力活动准则,制定了专门的居家运动锻炼推荐标准,大多数机构推荐使用在线运动课程或移动应用程序,表1总结了这些机构的主要建议。以家庭为基础的运动方式包括了有氧运动、力量锻炼、柔韧及平衡练习等。有氧运动可以通过使用楼梯和斜坡、家用设备或者一些徒手运动来进行;力量锻炼可以使用自身重量或简单家用负重物品,通过重复多次、多组以达到锻炼肌肉的目的;瑜伽、体操、伸展运动等柔韧及平衡练习也推荐进行。
当前,我国疫情进入常态化防控期,人们可以在社区、公园、体育场馆等地方进行体力活动。应遵循体力活动指南建议,即每周150 min中等强度或75 min高强度体力活动,或两者兼而有之;每周进行2 d及以上主要肌肉群的锻炼[102]。5~17岁儿童青少年推荐每天至少有60 min的中等强度以上的体力活动,每周至少保持3次增强肌肉和骨骼的活动[103]。佩戴口罩是COVID-19流行期间的关键防控措施,近期媒体连续报道了多起学校体育复课后运动型猝死事件,学生运动时佩戴口罩是否与猝死相关尚不确定,但运动时口罩降低了人体对氧气的吸收效率,增加呼吸阻力[104],因此,运动锻炼时不推荐佩戴口罩,保持社交距离即可。COVID-19流行期间,运动锻炼时的社交“安全距离”需要从静态1m增加到2 m;运动时产生的空气流动范围更大,最近的模型表明,直径2 m内的“气泡”形状随着运动而改变,而跑步或骑车的安全距离需要增加到5 m[105]。
4 展望
长期以来,全球一直在与体力活动不足和久坐行为作斗争。据WHO数据统计,在15岁或以上的人群中,31%的人缺乏运动,每年约有3 200 000人死于这种不健康的生活方式[33]。COVID-19暴发和流行,对全球人类健康造成前所未有的威脅,目前对这种疾病还没有特效药物或治疗方法,居家隔离与控制外出是一个限制病毒广泛传播最基本的疫情防控措施。然而,持续的社交隔离导致的体力活动不足会降低人的器官系统抵御病毒感染的能力,对免疫力、呼吸、心血管、肌肉骨骼系统以及心理造成损害。体力活动不足可能对人类健康造成“第二次”威胁,如果存在潜在的健康风险,则可能更容易感染COVID-19或感染后症状加重。因此,居民保持体力活动对于COVID-19流行期间疫情的防控具有重要作用。
目前,由于缺乏随机对照试验(RCT)研究,尚不能充分评估体力活动对COVID-19感染者死亡率和发病率的影响,需要进一步研究来证实。随着疫情的变化,有必要进行COVID-19患者的回顾性研究,以确定体力活动是否与SARS-CoV-2感染或COVID-19的结局有关。Ozemek 等对380 000名社区成年人回顾性队列研究发现,经年龄、性别及各种生活方式因素调整后,体力活动不足者COVID-19发病率更高(相对危险度1.32),提示了体力活动与COVID-19的关联性[33]。体力活动与COVID-19的流行病学研究,可以帮助决策者更好地了解COVID-19流行的影响因素以及相应防控措施的利弊。鉴于体力活动不足对人的健康产生的危害以及进行体力活动对疫情的积极防控作用,一些体育与卫生健康组织都相应行动起来,呼吁公众在COVID-19流行期间参与体力活动,并提出指导建议。中国国家体育总局积极倡导居家科学健身,在疫情初期就推出居家锻炼全年龄方案;美国运动医学会发布了COVID-19期间保持身体活跃的建议[107];美国疾病控制和预防中心发布了抗击体力活动不足的战略[109],COVID-19流行期间应推广体力活动,减少久坐。
参考文献:
[1] World Health Organization. Emergencies diseases novel-coronavirus-2019 situation- reports [EB/OL]. (2020-05-30)[2020-09-26]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
[2] HAN Q, LIN Q, JIN S, et al. Coronavirus 2019-nCoV: a brief perspective from the front line[J]. Journal of Infection, 2020, 80(4): 373.
[3] HELLEWLL J, ABBOTT S, GIMMA A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts[J]. The Lancet Global Health, 2020, 8(4): 488.
[4] LAU H, KHOSRAWIPOUR V, KOCBACH P, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China[J]. Journal of Travel Medicine, 2020, 27(3): 37.
[5] WELLS C R, SAH P, MOGHADAS S M, et al. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak[J]. Proceedings of the National Academy of Sciences, 2020,117(13): 7504.
[6] LIPPI G, HENRY B M, BOVO C, et al. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19)[J]. Diagnosis, 2020, 7(2): 85.
[7] WOODS J , HUTCHINSON N T , POWERS S K , et al. The COVID-19 pandemic and physical activity[J]. Sports Medicine and Health Science, 2020, 2(2): 55.
[8] World Health Organization. Stay physically active during self-quarantine [EB/OL].(2020-03-30)[2020-09-26]. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-gu-idance/stay-physically-active-during-self-quarantine.
[9] 岳建軍,龚俊丽,贝迎九,等. 体力活动生命体征:运动是良医的核心、体医融合的支点[J]. 成都体育学院学报,2018, 44(6): 116.
[10] DONOGHUE M, HSIEH F, BARONAS E, et al. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9[J]. Circulation Research, 2000, 87(5): e1.
[11] 崔立建, 刘瑞霞,王艳,等. ACE2-Ang(1-7)-Mas轴的生物学功能及其下游信号通路[J]. 基础医学与临床, 2014,34(12): 1718.
[12] ZHOU P, YANG X, WANG X, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin[J]. Nature, 2020, 579(7798): 270.
[13] WU C, ZHENG M. Single-cell RNA expression profiling shows that ACE2, the putative receptor of Wuhan 2019-nCoV, has significant expression in the nasal, mouth, lung and colon tissues, and tends to be co-expressed with HLA-DRB1 in the four tissues[EB/OL]. (2020-02-02)[2020-06-18]. https://www.preprints.org/manuscript/202002.0247/v1.
[14] 柴彦,郭喆,方奕鹏,等. ACE2在冠状病毒病-19多器官损伤中的作用[J]. 临床急诊杂志,2020,21(5): 417.
[15] GURWITZ D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics[J]. Drug Development Research, 2020, 81(5): 537.
[16] IMAI Y, KUBA K, RAO S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure[J]. Nature, 2005, 436(7047): 112.
[17] 唐欣颖,匡泽民. 从机制谈ACE/ACE2、RAS抑制剂与COVID-19的关系[J]. 中国动脉硬化杂志,2020,28(5): 390.
[18] GORBALENYA A E, BAKER S C, BARIC R S, et al. The species severe acute respiratory syndrome-related coronavirus:classifying 2019-nCoV and naming it SARS-CoV-2[J]. Nature Microbiology, 2020, 5(4):536.
[19] 杨峰,刘妮,胡杰英,等. 新型冠状病毒肺炎患者4S呼吸康复指引[J]. 中华结核和呼吸杂志,2020(3): 180.
[20] ZHOU F, YU T, DU R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study[J]. The Lancet, 2020,395(10229):1054.
[21] WANG D, HU B, HU C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-Infected Pneumonia in Wuhan, China[J]. JAMA, 2020, 323(11): 1061.
[22] HUANG C, WANG Y, LI X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China[J]. The Lancet, 2020, 395(10223): 497.
[23] YANG X, YU Y, XU J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study[J]. The Lancet Respiratory Medicine, 2020,8(5): 475.
[24] 董毅, 李瑞. 運动与自然杀伤细胞抗病毒等功能的关系和机制[J]. 中国体育科技, 2020, 56(5): 3.
[25] SCHIJNS V, LAVELLE E C. Prevention and treatment of COVID-19 disease by controlled modulation of innate immunity[J]. European Journal of Immunology, 2020,50(7):932.
[26] NORRIS F H, FRIEDMAN M J, WATSON P J. 60,000 disaster victims speak: part II. summary and Implications of the disaster mental health research[J]. Psychiatry MMC, 2002, 65(3): 240.
[27] SLOVIC P. Perception of risk[J]. Science, 1987, 236(4799): 280.
[28] LAI J, MA S, WANG Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019[J]. JAMA Network Open, 2020, 3(3): e203976.
[29] NETO M L R, ALMEIDA H G, ESMERALDO J D A, et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak[J]. Psychiatry Research, 2020(288):112972.
[30] LI S, WANG Y, XUE J, et al. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active weibo users[J]. International Journal of Environmental Research and Public Health, 2020, 17(6): 2032.
[31] STANTON R, TO Q G, KHALESI S, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults[J]. International Journal of Environmental Research and Public Health, 2020, 17(11): 4065.
[32] SHI L, LU Z A, QUE J Y, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic[J]. JAMA Network Open, 2020, 3(7): e2014053.
[33] OZEMEK C, LAVIE C J, ROGNMO O. Global physical activity levels - need for intervention[J]. Progress in Cardiovascular Diseases, 2019, 62(2): 102.
[34] PECANHA T, GOESSLER K F, ROSCHEL H, et al. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease[J]. American Journal of Physiology-Heart and Circulatory Physiology, 2020, 318(6): H1441.
[35] BRUUNSGAARD H. Physical activity and modulation of systemic low-level inflammation[J]. Journal of Leukocyte Biology, 2005, 78(4): 819.
[36] DRES M, DEMOULE A. Diaphragm dysfunction during weaning from mechanical ventilation: an underestimated phenomenon with clinical implications[J]. Critical Care, 2018, 22(1): 73.
[37] NUNESSILVA A, ROCHA G C, MAGALHAES D M, et al. Physical exercise and ACE2-angiotensin-(1-7)-mas receptor axis of the renin angiotensin system[J]. Protein and Peptide Letters, 2017, 24(9): 809.
[38] PENG W, HONG L, LIU G, et al. Prehypertension exercise training attenuates hypertension and cardiac hypertrophy accompanied by temporal changes in the levels of angiotensin II and angiotensin(1-7)[J]. Hypertension Research, 2019, 42(11): 1745.
[39] KAR S, GAO L, ZUCKER I H. Exercise training normalizes ACE and ACE2 in the brain of rabbits with pacing-induced heart failure[J]. Journal of Applied Physiology, 2010, 108(4): 923.
[40] FRANTZ E D C, PRODEL E, BRAZ I D, et al. Modulation of the renin-angiotensin system in white adipose tissue and skeletal muscle: focus on exercise training[J]. Clinical Science, 2018, 132(14): 1487.
[41] PRATA L O, RODRIGUES C R, MARTINS J M, et al. Original research: ACE2 activator associated with physical exercise potentiates the reduction of pulmonary fibrosis[J]. Experimental Biology and Medicine, 2017, 242(1): 8.
[42] HONCE R R, SCHULTZ-CHERRY S. Impact of obesity on influenza a virus pathogenesis, immune response, and evolution[J]. Frontiers in Immunology, 2019(10): 1071.
[43] LOUIE J K, ACOSTA M, WINTER K, et al. Factors associated with death or hospitalization due to pandemic 2009 influenza a (H1N1) infection in california[J]. JAMA, 2009, 302(17): 1896.
[44] CAMPBELL J, TURNER J E. Debunking the myth of exercise-induced immune suppression: redefining the impact of exercise on immunological health across the lifespan[J]. Frontiers in Immunology, 2018(9): 1.
[45] KOSTKA T, BERTHOUZE S E, LACOUR J R, et al. The symptomatology of upper respiratory tract infections and exercise in elderly people[J]. Medicine & Science in Sports & Exercise, 2000, 32(1): 46.
[46] KOSTKA T, PRACZKO K. Interrelationship between physical activity, symptomatology of upper respiratory tract infections, and depression in elderly people[J]. Gerontology, 2007, 53(4): 187.
[47] WOODS J A, KEYLOCK K T, LOWDER T W, et al. Cardiovascular exercise training extends influenza vaccine seroprotection in sedentary older adults: the immune function intervention trial[J]. Journal of the American Geriatrics Society, 2009, 57(12): 2183.
[48] SIMPSON R J, LOWDER T W, SPIELMANN G, et al. Exercise and the aging immune system[J]. Ageing Research Reviews, 2012, 11(3): 404.
[49] FISHER D, HEYMANN D. Q&A: the novel coronavirus outbreak causing COVID-19[J]. BMC Medicine, 2020, 18(1): 57.
[50] FLETCHER G F, LANDOLFO C, NIEBAUER J, et al. Promoting physical activity and exercise: JACC health promotion series[J]. Journal of the American College of Cardiology, 2018, 72(14): 1622.
[51] NIEMAN D C, WENTZ L M. The compelling link between physical activity and the bodys defense system[J]. Journal of Sport and Health Science, 2019, 8(3): 201.
[52] BERMON S, CASTELL L M, CALDER P C, et al. Consensus statement immunonutrition and exercise[J]. Exercise Immunology Review, 2017(23): 8.
[53] 王曉军. 太极拳对老年人NK细胞的影响[J]. 北京体育大学学报,2004,27 (5): 644.
[54] PEDERSEN B K, ULLUM H. NK cell response to physical activity: possible mechanisms of action[J]. Medicine and Science in Sports and Exercise, 1994, 26(2): 140.
[55] KHALEGHZADEH H, AFZALPOUR M E, AHMADI M M, et al. Effect of high intensity interval training along with oligopin supplementation on some inflammatory indices and liver enzymes in obese male wnistar rats with non-alcoholic fatty liver disease[J]. Obesity Medicine, 2020(17): 100177.
[56] TAHERICHADONESHIN H, CHERAGHBIRJANDI S, GOODARZY S, et al. The impact of high intensity interval training on serum chemerin, tumor necrosis factor-alpha and insulin resistance in overweight women[J]. Obesity Medicine, 2019(14): 100101.
[57] BARRETT B, HAYNEY M S, MULLER D, et al. Meditation or exercise for preventing acute respiratory infection: a randomized controlled trial[J]. Annals of Family Medicine, 2012, 10(4): 337.
[58] CERQUEIRA E, MARINHO D A, NEIVA H P, et al. Inflammatory effects of high and moderate intensity exercise-a systematic review[J]. Frontiers in Physiology, 2020(10): 1550.
[59] WARREN K J, OLSON M M, THOMPSON N J, et al. Exercise improves host response to influenza viral infection in obese and non-obese mice through different mechanisms[J]. PLOS One, 2015, 10(6):e0129713.
[60] WONG C M, LAI H K, OU C, et al. Is Exercise protective against influenza-associated mortality?[J]. PLOS One, 2008, 3(5):e2108.
[61] MATTHEWS C E, OCKENE I S, FREEDSON P S, et al. Moderate to vigorous physical activity and risk of upper-respiratory tract infection[J]. Medicine & Science in Sports & Exercise, 2002, 34(8): 1242.
[62] SIU E, CAMPITELLI M A, KWONG J C. Physical activity and influenza-coded outpatient visits, a population-based cohort study[J]. PloS One, 2012, 7(6):e39518.
[63] ZHOU G, LIU H, HE M, et al. Smoking, leisure-time exercise and frequency of self-reported common cold among the general population in northeastern China: a cross-sectional study[J]. BMC Public Health, 2018, 18(1): 294.
[64] NIEMAN D C, HENSON D A, AUSTIN M D, et al. Upper respiratory tract infection is reduced in physically fit and active adults[J]. British Journal of Sports Medicine, 2011, 45(12): 987.
[65] GRANDE A J, KEOGH J, HOFFMANN T C, et al. Exercise versus no exercise for the occurrence, severity and duration of acute respiratory infections[J]. Cochrane Database of Systematic Reviews, 2020(4):1.
[66] SLOAN C, ENGELS H, FAHLMAN M, et al. Effects of exercise on S-IGA and URS in postmenopausal women[J]. International Journal of Sports Medicine, 2013, 34(1): 81.
[67] BARRETT B, HAYNEY M S, MULLER D, et al. Meditation or exercise for preventing acute respiratory infection: a randomized controlled trial[J]. The Annals of Family Medicine, 2012, 10(4): 337.
[68] DAVIS J M, KOHUT M L, COLBERT L H, et al. Exercise, alveolar macrophage function, and susceptibility to respiratory infection[J]. Journal of Applied Physiology, 1997, 83(5): 1461.
[69] KAKANIS M, PEAKE J M, HOOPER S L, et al. The open window of susceptibility to infection after acute exercise in healthy young male elite athletes[J]. Exercise Immunology Review, 2010(13): 119.
[70] 鎮万源,蒋正文,王望才,等. 32例新型冠状病毒无症状感染者的临床特征分析[J]. 武汉大学学报(医学版),2021,42(1):23.
[71] NIELSEN H G, LYBERG T. Long-distance running modulates the expression of leucocyte and endothelial adhesion molecules[J]. Scandinavian Journal of Immunology, 2004, 60(4): 356.
[72] NIEMAN D C. Exercise, infection, and immunity[J]. International Journal of Sports Medicine, 1994, 15(S 3):S131.
[73] SHEPHARD R J, SHEK P N. Exercise, immunity, and susceptibility to infection: a j-shaped relationship?[J]. The Physician and Sportsmedicine, 1999, 27(6): 47.
[74] YANG Y, VERKUILEN J, ROSENGREN K S, et al. Effects of a traditional Taiji/Qigong curriculum on older adults immune response to influenza vaccine[J]. Medicine and Sport Science, 2008(52): 64.
[75] FALKENBERG R I, EISING C, PETERS M L. Yoga and immune system functioning : a systematic review of randomized controlled trials[J]. Journal of Behavioral Medicine, 2018, 41(4): 467.
[76] POWERS S K, BOMKAMP M, OZDEMIR M, et al. Mechanisms of exercise-induced preconditioning in skeletal muscles[J]. Redox Biology, 2020(35): 101462.
[77] SMUDER A J, MIN K, HUDSON M B, et al. Endurance exercise attenuates ventilator-induced diaphragm dysfunction[J]. Journal of Applied Physiology, 2012, 112(3): 501.
[78] SMUDER A J, MORTON A B, HALL S E, et al. Effects of exercise preconditioning and HSP72 on diaphragm muscle function during mechanical ventilation[J]. Journal of Cachexia, Sarcopenia and Muscle, 2019, 10(4): 767.
[79] FIGUEIREDO P H S, LIMA M M O, COSTA H S, et al. Effects of the inspiratory muscle training and aerobic training on respiratory and functional parameters, inflammatory biomarkers, redox status and quality of life in hemodialysis patients: a randomized clinical trial[J]. PLOS One, 2018, 13(7):e0200727.
[80] LOWDER T W, PADGETT D A, WOODS J A. Moderate exercise protects mice from death due to influenza virus[J]. Brain Behavior and Immunity, 2005, 19(5): 377.
[81] REBAR A L, STANTON R, GEARD D, et al. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations[J]. Health Psychology Review, 2015, 9(3): 366.
[82] KIECOLTGLASER J K, MCGUIRE L, ROBLES T F, et al. Emotions, morbidity, and mortality: new perspectives from psychoneuroimmunology[J]. Annual Review of Psychology, 2002, 53(1): 83.
[83] RIMMELE U, ZELLWEGER B C, MARTI B, et al. Trained men show lower cortisol, heart rate and psychological responses to psychosocial stress compared with untrained men[J]. Psychoneuroendocrinology, 2007, 32(6): 627.
[84] WOODS J HNT, POWERS S K. The COVID-19 pandemic and physical activity[J]. Sports Medicine and Health Science, 2020,2(2):55.
[85] AYLETT E, SMALL N, BOWER P. Exercise in the treatment of clinical anxiety in general practice-a systematic review and meta-analysis[J]. BMC Health Services Research, 2018, 18(1): 1.
[86] COONEY G, DWAN K, GREIG C A, et al. Exercise for depression[J]. Advances in Psychiatric Treatment, 2014, 20(1): 2.
[87] WIPFLI B, LANDERS D M, NAGOSHI C T, et al. An examination of serotonin and psychological variables in the relationship between exercise and mental health[J]. Scandinavian Journal of Medicine & Science in Sports, 2011, 21(3): 474.
[88] PASNEN T, TYRVAINEN L, KORPELA K. The relationship between perceived health and physical activity indoors, outdoors in built environments, and outdoors in nature[J]. Applied Psychology: Health and Well-being, 2014, 6(3): 324.
[89] PEDERSEN B K, BRUUNSGAARD H. Possible beneficial role of exercise in modulating low-grade inflammation in the elderly[J]. Scandinavian Journal of Medicine & Science in Sports, 2003, 13(1): 56.
[90] PETERSEN A M W, PEDERSEN B K. The anti-inflammatory effect of exercise[J]. Journal of Applied Physiology, 2005, 98(4): 1154.
[91] BONOW R O, FONAROW G C, OGARA P T, et al. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality[J]. JAMA Cardiology, 2020,5(7):751.
[92] INCIARDI R M, LUPI L, ZACCONE G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19)[J]. JAMA Cardiology, 2020,5(7):819.
[93] YANG C, JIN Z. An acute respiratory infection runs into the most common noncommunicable epidemic—COVID-19 and cardiovascular diseases[J]. JAMA Cardiology, 2020,5(7):743.
[94] KEMPS H, KRANKEL N, DORR M, et al. Exercise training for patients with type 2 diabetes and cardiovascular disease: what to pursue and how to do it. a position paper of the european association of preventive cardiology(EAPC)[J]. European Journal of Preventive Cardiology, 2019, 26(7): 709.
[95] KRANKEL N, BAHLS M, VAN CRAENENBROECK E M, et al. Exercise training to reduce cardiovascular risk in patients with metabolic syndrome and type 2 diabetes mellitus: how does it work?[J]. European Journal of Preventive Cardiology, 2019, 26(7): 701.
[96] CRISAFULLI A, PAGLIARO P, ROBERTO S, et al. Diabetic cardiomyopathy and ischemic heart disease: prevention and therapy by exercise and conditioning[J]. International Journal of Molecular Sciences, 2020, 21(8): 2896.
[97] OZEMEK C, LADDU D, LAVIE C J, et al. An update on the role of cardiorespiratory fitness, structured exercise and lifestyle physical activity in preventing cardiovascular disease and health risk[J]. Progress in Cardiovascular Diseases, 2018, 61: 484.
[98] RUIZ J R, HUYBRECHTS I, CUENCAGARCIA M, et al. Cardiorespiratory fitness and ideal cardiovascular health in European adolescents[J]. Heart, 2015, 101(10): 766.
[99] CASTRO-PIOERO J, PEREZ-BEY A, SEGURA-JIMENEZ V, et al. Cardiorespiratory fitness cutoff points for early detection of present and future cardiovascular risk in children: a 2-year follow-up study[C]. Mayo Clinic Proceedings, 2017: 1753.
[100] KODAMA S, SAITO K, TANAKA S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis[J]. Jama, 2009, 301(19): 2024.
[101] HEROUX M, JANSSEN I, LAM M, et al. Dietary patterns and the risk of mortality: impact of cardiorespiratory fitness[J]. International Journal of Epidemiology, 2010, 39(1): 197.
[102] World Health Organization. Global recommendations on physical activity for health (18-64 years old) [EB/OL]. (2011-12-01)[2020-06-18]. https://www.who.int/dietphysicalactivity/physical-activity-recommendations-18-64years.pdf?ua=1.
[103] World Health Organization. Global recommendations on physical activity for health(5-17 years old)[EB/OL]. (2011-12-01) [2020-06-18]. https://www.who.int/dietphysicalactivity/publications/physical-activity-recommendations-5-17years. pdf?ua=1.
[104] WU J, ZHA P. Mask is a double-edged sword in the fight against COVID-19 pandemic[J]. Available at SSRN 3563851, 2020:1.
[105] BLOCKEN B, MALIZIA F, DRUENEN VON T, et al. Towards aerodynamically equivalent COVID19 1.5 m social distancing for walking and running[EB/OL] .(2020-04-08)[2020-06-10]. http://www.urbanphysics.net/Social%20Distancing%20v20_White_Paper.pdf.
[106] 國家体育总局体育居家锻炼(全年龄方案)[EB/OL].(2020-02-12)[2020-05-10]. http://www.sport.gov.cn/n4/n15204/n15207/c942519/content.html.
[107] American College of Sports Medicine. Exercise is medicine[EB/OL].(2020-04-03)[2020-05-10]. https://www.exerciseismedicine.org/support_page.php/stories/?b=892.
[108] American Heart Association. Create a circuit home workout Infographic[EB/OL]. (2020-04-03)[2020-05-10].https://www.heart.org/en/healthy-living/fitness/getting-active/create-acircuit-home-workout.
[109] Centers for Disease Control and Prevention. Coronavirus disease 2019(Covid-19) daily life and coping[EB/OL]. (2020-04-01)[2020-05-10]. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fmanaging-stressanxiety.htm7.

