Integrated strategies for chemotherapy cycles in nasopharyngeal carcinoma patients: Real-world data from two epidemic centers guiding decision-making
Zejiang Zhan ,Yingying Huang ,Jiayu Zhou ,Zhuochen Cai ,Haoyang Huang ,Ying Deng ,Wenze Qiu,Xun Cao,Xi Chen,Chixiong Liang,Lulu Zhang,Xiang Guo,Taize Yuan,Xing Lyu
1Department of Nasopharyngeal Carcinoma,Sun Yat-sen University Cancer Center,the State Key Laboratory of Oncology in South China,Collaborative Innovation Center for Cancer Medicine,Guangdong Key Laboratory of Nasopharyngeal Carcinoma Diagnosis and Therapy,Guangzhou 510060,China;2 Department of Radiation Oncology,Affiliated Cancer Hospital and Institute of Guangzhou Medical University,Guangzhou 510095,China;3Department of Critical Care Medicine,Sun Yat-sen University Cancer Center,the State Key Laboratory of Oncology in South China,Collaborative Innovation Center for Cancer Medicine,Guangzhou 510060,China;4 Department of Radiation Oncology,Guangzhou Concord Cancer Center,Guangzhou 510045,China
Abstract Objective:Two cycles of induction chemotherapy (IC) followed by 2 cycles of platinum-based concurrent chemoradiotherapy (CCRT) (2IC+2CCRT) for locoregionally advanced nasopharyngeal carcinoma (LA-NPC) is widely adopted but not evidence-confirmed.This study aimed to determine the clinical value of 2IC+2CCRT regarding efficacy,toxicity and cost-effectiveness.Methods:This real-world study from two epidemic centers used propensity score matching (PSM) and inverse probability of treatment weighting (IPTW) analyses.The enrolled patients were divided into three groups based on treatment modality: Group A (2IC+2CCRT),Group B (3IC+2CCRT or 2IC+3CCRT) and Group C(3IC+3CCRT).Long-term survival,acute toxicities and cost-effectiveness were compared among the groups.We developed a prognostic model dividing the population into high-and low-risk cohorts,and survivals including overall survival (OS),progression-free survival (PFS),distant metastasis-free survival (DMFS) and locoregional relapse-free survival (LRRFS) were compared among the three groups according to certain risk stratifications.Results:Of 4,042 patients,1,175 were enrolled,with 660,419,and 96 included in Groups A,B and C,respectively.Five-year survivals were similar among the three groups after PSM and confirmed by IPTW.Grade 3-4 neutropenia and leukocytopenia were significantly higher in Groups C and B than in Group A (52.1% vs.41.5% vs. 25.2%;41.7% vs. 32.7% vs. 25.0%) as were grade 3-4 nausea/vomiting and oral mucositis (29.2% vs.15.0% vs. 6.1%;32.3% vs. 25.3% vs. 18.0%).Cost-effective analysis suggested that 2IC+2CCRT was the least expensive,while the health benefits were similar to those of the other groups.Further exploration showed that 2IC+2CCRT tended to be associated with a shorter PFS in high-risk patients,while 3IC+3CCRT potentially contributed to poor PFS in low-risk individuals,mainly reflected by LRRFS.Conclusions:In LA-NPC patients,2IC+2CCRT was the optimal choice regarding efficacy,toxicity and costeffectiveness;however,2IC+2CCRT and 3IC+3CCRT probably shortened LRRFS in high-and low-risk populations,respectively.
Keywords: Nasopharyngeal carcinoma;treatment modality;chemotherapy cycle;survival;toxicity;costeffectiveness;real world
Introduction
Head and neck cancers pose a heavy disease burden in China (1-3).Nasopharyngeal carcinoma (NPC) is a common head and neck malignant tumor originating from the nasopharyngeal mucosa epithelium.A total of 133,354 NPC patients were identified globally in 2020,and nearly half of the new cases were geographically distributed in China (3).The early symptoms of NPC lack specificity,leading to more than 70% of patients being in an aggressive stage at presentation (4).Platinum-based concurrent chemoradiotherapy (CCRT) regimens remain the mainstay treatment modality for these patients (5-7).
Previous studies have shown that both induction chemotherapy (IC) and adjuvant chemotherapy (AC) are clinically beneficial when combined with CCRT (8,9),with considerable overall survival (OS) rates reaching 92.0%-94.6% in 3 years and 80.8%-89.0% in 5 years (10-13).Patient compliance and treatment-related toxicities should be highlighted despite the improvement in survival.Compared with AC following CCRT (CCRT+AC),IC followed by CCRT (IC+CCRT) results in fewer treatmentinduced toxicities and has been deemed to be a more tolerable treatment modality (14).The IC regimens recommended in National Comprehensive Cancer Network (NCCN) guidelines and most commonly used in clinical practice are gemcitabine plus cisplatin (GP);docetaxel,cisplatin,and fluorouracil (TPF);cisplatin plus fluorouracil (PF);and docetaxel plus cisplatin (TP) (7).However,controversy remains in regard to the optimal number of integrated chemotherapy cycles administered in the setting of IC and CCRT.
The cumulative doses of platinum-based agents delivered during radiotherapy in NPC patients have been explored in various studies.For patients without administration of IC and AC,the optimal threshold of platinum agent for ideal efficacy was a cumulative dose of 200 mg/m² (15,16),which means that a delivery of 3 cycles of platinum-based agents during radiotherapy is essential when the dosing schedule is 80-100 mg/m² every 3 weeks.Of note,a high dose of platinum-based agents has been correlated with poor patient compliance and more aggressive toxicity profiles,such as vomiting and nausea,leading to only 56.0%-69.4%of patients completing three cycles of CCRT as required by the protocol in previous randomized controlled trials(RCTs) (13,17,18).Maiet al.made efforts to deintensify the chemoradiotherapy strategy in NPC patients and demonstrated that patients complied well with two cycles of concurrent cisplatin compared to three cycles and that two cycles were enough in certain populations (19).However,patients in this study underwent CCRT alone,and neither IC nor AC was used.Since IC plays an important role in improving patient survival,the cumulative doses and chemotherapy cycles during CCRT following IC have attracted interest from researchers.On the basis of IC,a cumulative dose of platinum-based agent of 200 mg/m² administered during radiotherapy did not yield a favorable survival,whereas 160 mg/m² might be enough for patients (20).This means that 2 cycles of CCRT may be optimal when the dosing schedule is 80-100 mg/m2every 3 weeks,whereas 3 cycles may be burdensome.
Nevertheless,the present RCTs regarding IC in NPC patients usually involved 3 cycles of IC followed by 3 cycles of CCRT (3IC+3CCRT) (10,13),which was deemed the standard modality.Notably,the 3IC+3CCRT modality has been shown to have a high dose intensity and poor patient compliance,resulting in only 30.0%-38.9% of patients completing three cycles of concurrent platinum agents,as in the initial protocol design (10,13).Our previous RCT on the PF regimen (11) comparing lobaplatin and cisplatin confirmed its clinical value with satisfactory long-term patient survival,consistent with relevant studies (10,12).It is worth noting that 91.3% and 84.3% of patients in the experimental and control groups,respectively,completed the protocol-assigned cycles of CCRT,which was much higher than the 30.0%-38.9% reported in GP and TPF regimen-related RCTs (10,13).However,following the release of our PF regimen-related RCT,Cavalieri and Licitra (21) argued that the treatment modality of 2 cycles of IC followed by 2 cycles of CCRT (2IC+2CCRT)conducted in this trial was not the standard strategy compared to 3IC+3CCRT,which was supported by solid evidence from previous RCTs and was recommended by NCCN guidelines (7).It cannot be ignored that some researchers have revealed that more courses of IC do not guarantee an efficacy benefit,and instead,the toxicity profiles are aggressive,whereas 2 cycles may be the optimal number of cycles (22,23).
3IC+3CCRT is the standard treatment modality at present,while 2IC+2CCRT may have guaranteed efficacy,tolerable toxicity and a reduced burden,as it is widely adopted in clinical practice,although it has not been proven by direct comparison.Controversy remains in regard to whether 2IC+2CCRT is a deintensified alternative strategy for locoregionally advanced NPC (LANPC),and evidence is lacking since no studies have been conducted focusing directly on the clinical value of the 2IC+2CCRT modality in these patients.Further determination of the exact role of the 2IC+2CCRT modality in NPC patients is imperative.Therefore,by performing a retrospective,propensity score-matched(PSM) and inverse probability of treatment weighting(IPTW) analysis,this study determined the clinical value of the 2IC+2CCRT integrated treatment modality in LANPC patients based on real-world data from two epidemic centers.
Materials and methods
This was a retrospective study that involved PSM and IPTW analyses of real-world data from two epidemic centers,namely,the Sun Yat-sen University Cancer Center and the Affiliated Cancer Hospital &Institute of Guangzhou Medical University.The data for the enrolled patients were extracted between Janaury 2012 and December 2016.Figure 1shows the process of patient screening.The Research Ethics Committee of the Sun Yatsen University Cancer Center (No.SL-B2022-697-01)granted the approval for conducting this study and informed consent was exempted due to the retrospective design.

Figure 1 Flowchart of patient selection.LA-NPC,locoregionally advanced nasopharyngeal carcinoma;RT,radical radiotherapy;IC,induction chemotherapy;AC,adjuvant chemotherapy;CCRT,concurrent chemoradiotherapy;PSM,propensity score matching;IPTW,inverse probability of treatment weighting;NA,not available.Variables for PSM and IPTW matching were age,gender,T stage,N stage,clinical stage,LDH level and EBV-DNA status.
Patient population
For all patients,the clinical stage was restaged by senior doctors according to the American Joint Committee on Cancer/Union for International Cancer Control(AJCC/UICC) Classification (2017,8th edition).The pathological type was determined following the World Health Organization (WHO) histological classification of NPC,and the performance status was confirmed by the Eastern Cooperative Oncology Group (ECOG) standard.The main inclusion criteria were as follows: 1)pathologically confirmed WHO type II or III NPC;2)stage III or IVa disease;3) ECOG performance status of 0-1;and 4) treatment modality of IC+CCRT.The main exclusion criteria were as follows: 1) a history or cooccurrence of other malignant tumors;2) neither 2 nor 3 IC cycles;3) incomplete clinical data (including those with no follow-up after radical radiotherapy);4) additional administration of anti-epidermal growth factor receptor(anti-EGFR) monoclonal antibody therapies,such as cetuximab or nimotuzumab;5) one cycle or no platinumbased single-agent CCRT;or 6) severe heart,liver,kidney,lung function impairment and other diseases.
Treatment
Chemotherapy was administered every 3 weeks per cycle in both the IC and CCRT settings.For IC,the enrolled patients were administered 2-3 cycles of the regimens recommended by the NCCN guidelines (7),such as GP,TPF,PF and TP.For CCRT,2-3 cycles of a platinumbased single agent were administered.The dosing schedules of IC and CCRT were determined by the investigators according to the NCCN guidelines (7).Based on the integrated treatment modality of chemotherapy cycles in the settings of IC and CCRT,three groups were defined,namely,Group A (2IC+2CCRT),Group B(3IC+2CCRT or 2IC+3CCRT) and Group C(3IC+3CCRT).
In terms of radiotherapy,simultaneous intensitymodulated radiotherapy (IMRT) was performed for all patients.The target volumes were delineated according to the Sun Yat-sen University Cancer Center institutional treatment protocol (24).Gross tumor volumes (GTVs)were determined by computed tomography (CT) and magnetic resonance imaging (MRI),physical examination,and nasal endoscopy results.The doses to the nasopharynx GTV (GTVnx) and lymph node GTV (GTVnd) were 68-70 Gy.The doses to the clinical target volume (CTV)were ≥54 Gy.Irradiation to the GTVnx,GTVnd,and CTV was administered once a day 5 consecutive times per week,with a total fraction of 30-33.
Outcomes
The aim of this study was to explore the clinical value of the 2IC+2CCRT treatment modality by analyzing patient survival,safety profiles and cost-effectiveness.Hence,both long-term survival data and peri-treatment acute toxicity profiles were collected.OS was defined as the interval from the date of diagnosis to mortality from any cause or the last follow-up.Progression-free survival (PFS),distant metastasis-free survival (DMFS) and locoregional relapsefree survival (LRRFS) were defined as the time from the date of diagnosis to disease progression,distant metastasis,or locoregional relapse,respectively.Peri-treatment acute toxicity profiles were documented and graded in accordance with the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE,version 4.0).
Follow-up
After the completion of antitumor therapy,patients were followed up regularly.Subsequent follow-up of patients was performed at an interval of 3 months in the first 2 years,every 6 months in years 3-5,and every year thereafter.Follow-up visits included physical examination,chest radiography and/or CT,abdominal ultrasound and/or CT,electronic nasopharyngoscopy,head and neck MRI,and positron emission computed tomography (PET)whenever necessary.
Statistical analysis
PSM analysis (25) was performed to balance the potential prognostic factors in different competing groups using the R package “TriMatch” (26).A caliper value of 0.1 was set,and PSM was performed with a one-to-one nearest neighbor matching algorithm.Notably,PSM may not be able to match all samples successfully,so the loss of sample size caused by matching cannot be ignored,and it is even impossible to determine whether the matched samples can represent the original research samples.Owing to an inevitable outflow of enrolled patients after performing PSM,we performed IPTW analysis to address this deficiency to some extent (27).Using the R package“MASS” (28),we built logistic regressions to estimate the propensity score (PS) of each sample belonging to the target group,utilizing covariates including age,gender,histological type,AJCC stage,smoking status,lactate dehydrogenase (LDH) level,Epstein-Barr virus (EBV)-DNA status,and body mass index (BMI).We then computed the inverse of the probability of being in the observed group as the weight for each participant,consistent with what had been done in the study of Chesnaye and Kishan (29,30).Equilibrium among matched participants (Group Avs.Group Bvs.Group C) was evaluated by testing for differences in covariates using the Chi-square test and Fisher’s exact test where appropriate as well as the acute toxicity profiles.
Survival was analyzed and compared using the Kaplan-Meier method and the log-rank test,and the results for competing groups after performing PSM and IPTW analyses were used for mutual verification.Univariate and multivariate analyses by the Cox proportional hazards model were performed to identify potentially important prognostic factors.We used the Forward:LR method for multivariate analysis to explore which variables were ultimately left in the equation and deemed independent prognostic factors.Based on the independent prognostic factors screened out by multivariate Cox regression analysis,we developed a prognostic model to divide the population into high-and low-risk cohorts (31).Survival was compared among the three groups (Group A,Group B and Group C) according to certain risk stratifications to explore the potential individuals who benefited in each group.The expenditure of medical care cannot be ignored(32).We constructed a Markov model to evaluate the cost and health benefits (33).A series of parametric survival models,including Weibull,log-normal,log-logistic,Gompertz,Gamma and Exponential,were considered in fitting the survival probability function.However,for each situation,only the distribution with the lowest Bayesian information criterion (BIC) values was selected(Supplementary Table S1).The utility for patients with PFS or progressive disease (PD) status was set at 0.76 and 0.57,respectively (34).The total medical costs,namely,PFS with/without complications,including lab tests,medical imaging,chemotherapy,radiotherapy,supportive care and adverse event-related costs,are summarized inSupplementary Table S2.Cost-effective analysis was conducted using TreeAge Pro 2011 software (Version 2011;TreeAge Software,Williamstown,MA,USA).Probabilistic sensitivity analysis was performed to calculate the cost-effective probability under different willingnessto-pay (WTP) thresholds.According to the WHO criteria,we applied $33,507.3 as a WTP threshold,which was 3 times per capita GDP of China in 2021.IBM SPSS Statistics (Version 26.0;IBM Corp.,New York,USA) and R software (Version 3.6.3;R Foundation for Statistical Computing,Vienna,Austria) were applied for statistical analyses.P<0.050 denotes significant differences.For toxicity profiles between groups,Bonferroni correction was applied for correction of alpha type I error.The correction test level alpha was=0.050/3=0.017;thus,if P<0.017,we considered that there was a difference between the two groups.
Results
Patient characteristics
As shown inFigure 1,a total of 4,042 newly diagnosed LANPC patients from the Sun Yat-sen University Cancer Center and the Affiliated Cancer Hospital &Institute of Guangzhou Medical University between January 2012 and December 2016 were screened.After conforming to the inclusion and exclusion criteria,1,175 patients were finally identified for subsequent analysis,with 660,419 and 96 patients in Group A,Group B and Group C,respectively.A total of 2,867 patients were excluded for the following reasons: 1) no administration of IC (n=1,163);2) neither 2 nor 3 IC cycles (n=277);3) received AC or anti-EGFR monoclonal antibody therapies,such as cetuximab or nimotuzumab (n=482);4) one cycle or no platinum-based single-agent CCRT (n=785);5) a history or co-occurrence of other malignant tumors (n=84);or 6) incomplete clinical data (including those with no follow-up after radical radiotherapy) or coexisting severe heart,liver,kidney,lung function impairment and other diseases (n=76).PSM analysis was performed in a 4:4:1 ratio,with 174,161 and 96 patients left in the PSM cohort of Group A,Group B and Group C,respectively,after matching.For the IPTW cohort,none of the enrolled patients were excluded after performing IPTW analysis.The matching variables for PSM and IPTW analyses were age,gender,T stage,N stage,clinical stage,LDH level and EBV-DNA status.Patient characteristics in the PSM cohort and IPTW cohort were well balanced among the groups (Table 1).
Survival analysis
Patient survival for the PSM cohort and IPTW cohort was assessed,thus minimizing the potential prognostic factors in different competing groups.
A total of 431 patients remained in Group A,Group B and Group C after performing PSM.The median followup time of PSM population was 77 (7-120) months,and the 5-year OS,PFS,DMFS and LRRFS rates were 93.9%,83.7%,91.4% and 90.9%,respectively.The OS,PFS,DMFS and LRRFS rates of patients in Group Avs.Group Bvs.Group C were 93.4%vs.93.3%vs.94.6%,82.9%vs.87.0%vs.79.8%,91.1%vs.92.3%vs.90.5% and 89.2%vs.94.5%vs.88.1%,respectively,with no significant difference in the 5-year survival rates among the groups(Supplementary Figure S1).
For the IPTW cohort,none of the enrolled patients were omitted after performing IPTW analysis.With a median follow-up time of 75 (4-120) months,the 5-year OS,PFS,DMFS and LRRFS rates were 93.7%,81.8%,90.1% and 90.7%,respectively.The OS,PFS,DMFS and LRRFS rates of patients in Group Avs.Group Bvs.Group C were 93.3%vs.93.3%vs.94.1%,80.6%vs.84.1%vs.80.6%,89.4%vs.91.0%vs.89.2% and 89.6%vs.92.9%vs.90.3%,respectively,showing similar 5-year survival rates among the groups (Supplementary Figure S2).
Univariate and multivariate survival analyses
Univariate and multivariate survival analyses were performed in the whole study population of 1,175 patients.
In univariate analysis,age,T stage,N stage,clinical stage,smoking and LDH level were identified as prognostic factors of OS.Gender,histology,T stage,N stage,clinical stage and smoking were prognostic factors of PFS.Gender,N stage,clinical stage,smoking and LDH level were identified as prognostic factors of DMFS (Table 2).
Variables that were statistically significant in univariate analysis and those that were clinically considered to have an impact on prognosis were subsequently included in the multivariate analysis.Finally,all baseline variables were included in the multivariate analysis.The results showed that age,smoking history,LDH level and EBV-DNA status were independent prognostic factors of OS.Histology,T stage,N stage and clinical stage were independent prognostic factors of PFS.N stage and clinical stage were independent prognostic factors of DMFS(Figure 2).
Prognostic stratifications
A prognostic model was constructed using the statistically significant variables in multivariate Cox regression.The cutoff values used to divide the whole population into highand low-risk cohorts were defined by the median value of probability points.Figure 3shows that the lower risk group exhibited a better prognosis,represented by higher OS,LRRFS,DMFS and PFS (all P<0.050).Subsequently,survival was compared among the three groups according to certain risk stratifications.No statistically significant difference in the OS,LRRFS,DMFS and PFS outcomes among different groups was observed,either in the highrisk or low-risk cohort.However,2IC+2CCRT tended to be associated with a shorter PFS in high-risk patients(Group Avs.Group Bvs.Group C: 75.1%vs.80.5%vs.80.4%),while 3IC+3CCRT potentially contributed to a poor PFS in low-risk individuals (Group Avs.Group Bvs.Group C: 86.4%vs.86.6%vs.79.3%).PFS differences were mainly reflected by LRRFS (high-risk cohort: Group Avs.Group B: 86.1%vs.92.0%,P=0.059;low-risk cohort:Group Avs.Group C: 93.2%vs.85.5%,P=0.093)(Figure 3).
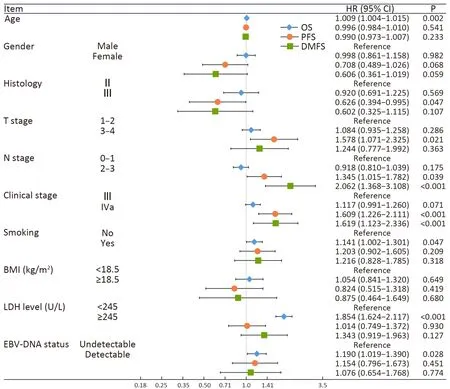
Figure 2 Multivariate analysis of OS,PFS and DMFS in the whole patient population.OS,overall survival;PFS,progression-free survival;DMFS,distant metastasis-free survival;BMI,body mass index;LDH,lactate dehydrogenase;EBV,Epstein-Barr virus;HR,hazard ratio;95% CI,95% confidence interval.
Toxicity profiles
Both acute hematologic and nonhematologic toxicity profiles among groups were compared in the whole study population of 1,175 patients.
For hematologic toxicities,grade 3-4 leukocytopenia and neutropenia in Group A were more tolerable than those in Groups B and C [25.0%vs.32.7%vs.41.7%;25.2%vs.41.5%vs.52.1%;P values between Groups A and B and Groups A and C showed significant differences (P=0.006 and P=0.001)].No significant differences were found in incidences of grade 3-4 anemia and thrombocytopenia among the three groups (P>0.017) (Table 3).
In terms of nonhematologic toxicities,grade 3-4 nausea/vomiting was more common in Group C and Group B than in Group A [29.2%vs.15.0%vs.6.1%,all P values between groups denoted significant differences(P=0.001,P<0.001 and P<0.001)].Grade 3-4 radiationinduced oral mucositis tended to be more aggressive in Groups C and B than in Group A [32.3%vs.25.3%vs.18.0%,P values between Groups A and B,Groups A and C showed significant differences (P=0.004 and P=0.001)].Incidences of liver and kidney function impairment among the groups were comparable,showing no significant differences between groups (P>0.017) (Table 3).
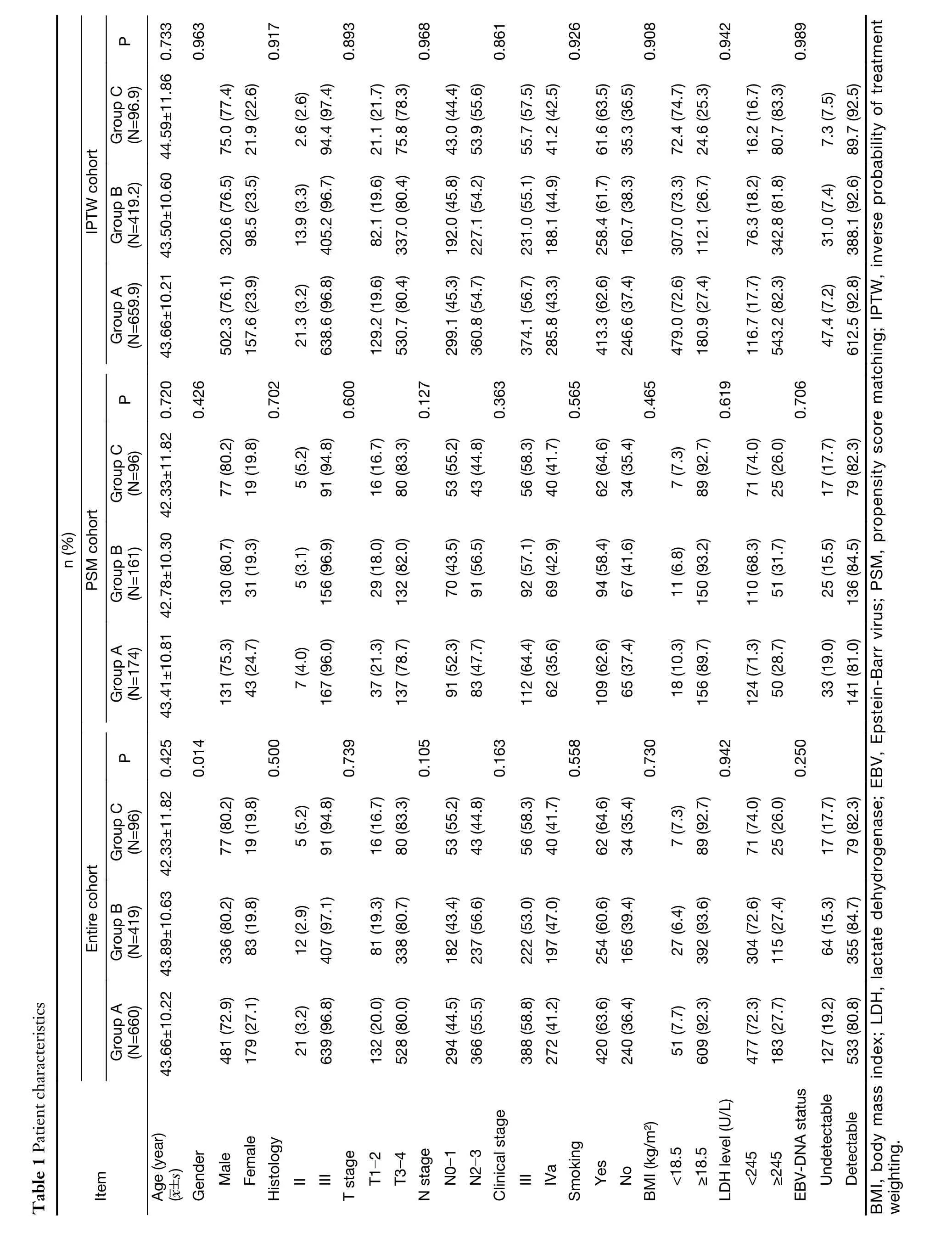
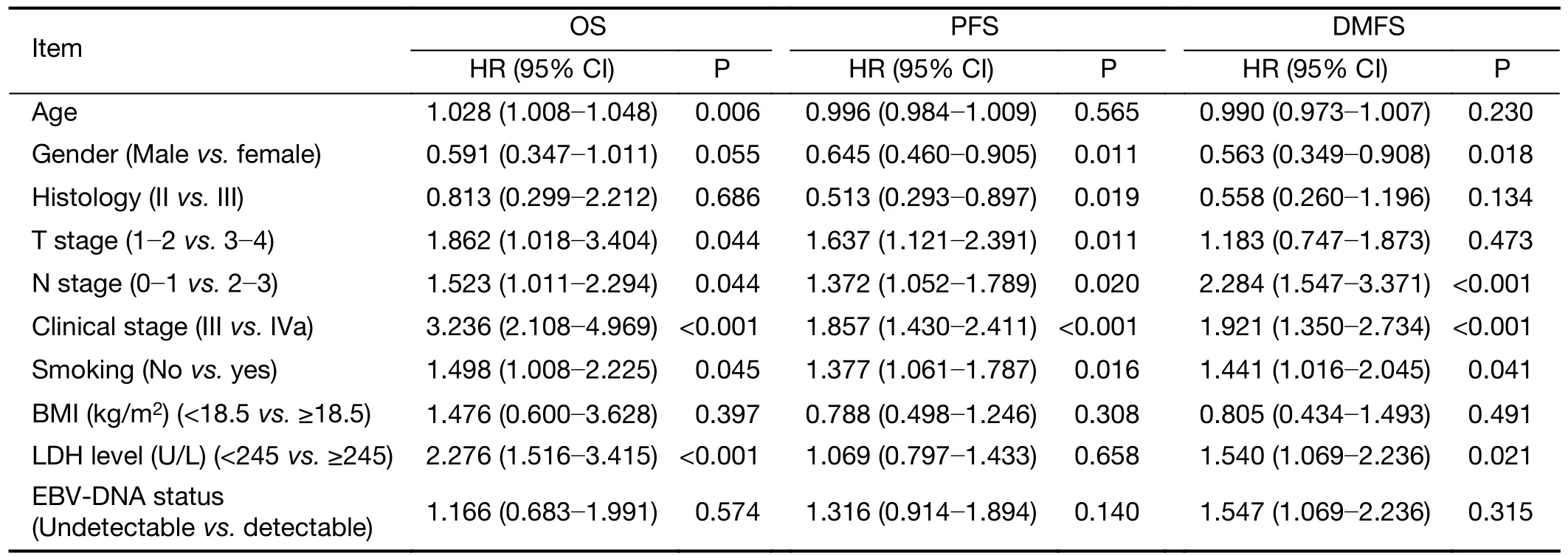
Table 2 Univariate analysis of OS,PFS and DMFS in whole patient population
Cost-effectiveness analysis
The initial cost and increment cost per cycle are summarized inSupplementary Table S2.Over a 5-year horizon,the 2IC+2CCRT modality had the lowest medical cost compared with 3IC+2CCRT or 2IC+3CCRT and 3IC+3CCRT ($20,186vs.$21,248vs.$22,356,respectively),while the quality-adjusted life year (QALY)remained similar (3.579vs.3.576vs.3.516,respectively).The cost-effectiveness acceptability curve indicated that the 2IC+2CCRT strategy remained the most cost-effective at any WTP threshold,and the probability of the 2IC+2CCRT strategy remaining cost-effective was 98.6%when the WTP threshold was set at $33,507.3 (Figure 4).

Table 3 Adverse events during treatment in whole population
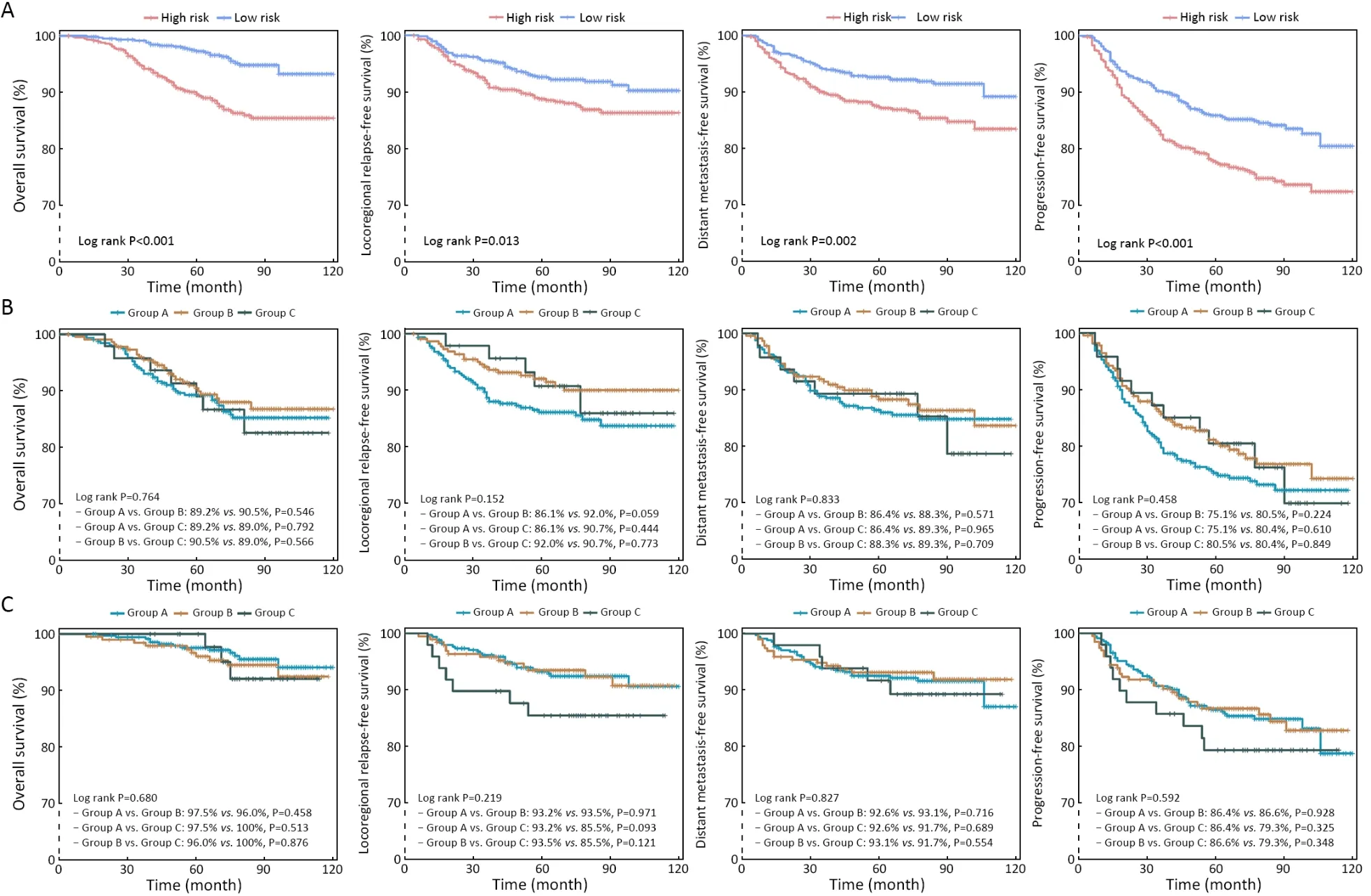
Figure 3 Survival analysis by risk stratification (A) and comparisons among three groups in high-(B) and low-risk (C) populations.
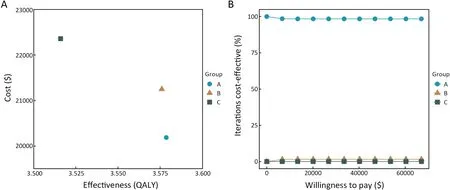
Figure 4 Cost-effectiveness analysis among groups.QALY,quality-adjusted life year.
Discussion
To our knowledge,the present study is the first to ascertain the clinical value of the integrated chemotherapy modality of 2IC+2CCRT directly compared with the 3IC+3CCRT and 3IC+2CCRT or 2IC+3CCRT modalities in NPC patients.Through real-world data from two epidemic centers and by performing PSM and IPTW analyses,the superiority of the 2IC+2CCRT modality in safety profiles and cost-effectiveness was revealed;moreover,this modality had guaranteed efficacy in terms of patient survival,thus potentially serving as a promising treatment choice.Further explorations showed that 2IC+2CCRT tended to be associated with a shorter LRRFS in high-risk patients,while 3IC+3CCRT potentially contributed to a poor LRRFS in low-risk individuals.Decision-making in clinical practice and the design of future RCTs could be carried out on the basis of these findings.
At present,IC+CCRT is the most commonly used and recognized treatment modality in patients with LA-NPC,and evidence confirms the efficacy of this treatment when compared with CCRT alone (10,13,17).Previous RCTs concerning IC for NPC patients mostly focused on the 3IC+3CCRT modality (10,13).Disappointingly,the vast majority of these patients could not withstand the full course of chemotherapy due to severe toxicities,resulting in merely 30.0%-38.9% of patients completing the total protocol-designed chemotherapy cycles.Nevertheless,most ongoing RCTs (e.g.,ChiCTR1800016613,ChiCTR2100051510,NCT03306121,and NCT0443 7329) are designed on the basis of 3IC+3CCRT,while some are designed on the basis of 3IC+2CCRT (e.g.,ChiCTR2200060136 and NCT03503136).The treatment modality of 2IC+2CCRT is clinically recognized and commonly used in the real world because of its remarkable efficacy and tolerability;however,no direct comparisons to the modalities prevailing in trial designs,such as 3IC+3CCRT and 3IC+2CCRT or 2IC+3CCRT,have been performed.The present work exploring the clinical value of the 2IC+2CCRT modality may guide decisionmaking and trial designs in terms of integrated strategies for chemotherapy cycles.
To minimize the potential prognostic factors in different competing groups,this study employed both PSM and IPTW analyses to balance the baseline characteristics of paired groups,consistent with the methods previously applied in Grool and his colleagues’ work (35).First,we performed PSM analysis among the three groups,namely,the clinically recognized but not evidence-confirmed treatment modality of 2IC+2CCRT,the 3IC+2CCRT or 2IC+3CCRT modality and the 3IC+3CCRT modality (the most favored modality in trial designs).Subsequently,we performed IPTW analysis,and the results showed that the 5-year OS,PFS,DMFS and LRRFS rates of the competing groups were comparable to those of the PSM cohort.The PFS was comparable to that in a previous study,while OS was better in the present work (11),which may be attributed to superior DMFS in this study.Lv and his colleagues’ work (11),which adopted the 2IC+2CCRT modality in LA-NPC patients,compared cisplatin and lobaplatin in the PF regimen,and the results showed that the 5-year OS was 88.2%-89.0% in all enrolled populations.This was worse than what we found in this study,in which OS of the 2IC+2CCRT group was 93.7%-93.9% in the PSM cohort and IPTW cohort.Of particular note,clinical stage and N stage are closely related to patient prognosis (36,37).More patients with a better prognosis in terms of clinical stage and N stage were identified in our present work than in Lv and his colleagues’ study (11).This may explain why patients in our study had better survival rates.In contrast to the 3IC+3CCRT and 3IC+2CCRT or 2IC+3CCRT modalities,the 2IC+2CCRT modality demonstrated similar survival despite its lower treatment intensity.It is encouraging that patients could achieve comparable antitumor activity without having to undergo highly intensive treatment.In multivariate analysis,we found that age,smoking,LDH level and EBV-DNA status were independent prognostic factors of OS,consistent with previous work (38-41).
To explore the potential individuals who benefited from each group (Group A,Group B and Group C),we compared survival among the three groups in certain risk stratifications generated from a prognostic model.The results suggested that survival was comparable among different groups,regardless of risk stratification.However,2IC+2CCRT and 3IC+3CCRT probably shortened LRRFS in high-and low-risk populations,respectively,although no significant difference was observed.This result indicated that high-risk patients may benefit from intensive treatment,while low-risk individuals should be introduced to a deintensified strategy.
Regarding treatment-related toxic effects,efforts have been made by many researchers to reduce toxicity and enhance therapeutic compliance in NPC patients,such as replacing cisplatin-based regimens with other platinumbased regimens (11,18,41) and deintensified chemoradiotherapy (19).Our present real-world study explored the integrated strategies of chemotherapy cycles in NPC patients for the first time and revealed that the deintensified modality of 2IC+2CCRT resulted in fewer grade 3-4 acute hematologic and nonhematologic toxicities.Neutrophils serve as the body’s first-line defense,and the decline in neutrophil count renders the body vulnerable to infections (42).Febrile neutropenia is one of the most serious conditions of neutrophil count decline and is characterized by fever during a period of significant neutropenia (42).It is a common complication in patients undergoing antitumor therapies,and hence,avoiding grade 3-4 neutropenia and leukocytopenia as much as possible is of utmost importance.In the 2IC+2CCRT group,manageable grade 3-4 neutropenia occurred,whereas its incidence was much higher in the 3IC+2CCRT or 2IC+3CCRT and 3IC+3CCRT groups (25.2%vs.41.5%vs.52.1%);the same result was found for the frequency of grade 3-4 leukocytopenia (25.0%vs.32.7%vs.41.7%).Nonhematologic toxicities such as radiation-induced oral mucositis and gastrointestinal reactions seriously affect the subjective experience and treatment compliance of patients.Therefore,a modality with fewer toxicities and guaranteed efficacy would surely be popular with patients and oncologists.Of special note,3IC+3CCRT is an intensified modality accompanied by unacceptable safety profiles,resulting in only 30.0%-38.9% of patients completing the protocol-assigned chemotherapies in the relevant RCTs(10,13).In Lv and his colleagues’ RCT employing the 2IC+2CCRT modality (11),the toxic effects were manageable,ensuring that most of the patients(84.3%-91.3%) completed the protocol-assigned chemotherapies.Our present study made a direct comparison among 2IC+2CCRT,3IC+2CCRT or 2IC+3CCRT and 3IC+3CCRT,showing that grade 3-4 nausea/vomiting was less frequent in the 2IC+2CCRT group,while it was notable in the 3IC+2CCRT or 2IC+3CCRT and 3IC+3CCRT groups (6.1%vs.15.0%vs.29.2%),as was grade 3-4 radiation-induced oral mucositis(18.0%vs.25.3%vs.32.3%).These results may explain why only a small number of patients could complete the treatment of 3IC+3CCRT modality to some extent.
Inevitably,some limitations should be acknowledged for this real-world analysis.First,this study was a retrospective,real-world analysis based on data from two epidemic cancer centers.Potential prognostic factors in different competing groups might influence survival between groups;hence,we applied PSM and IPTW analyses to better compensate for this deficiency.Additionally,objective toxic effects,such as gastrointestinal reactions,were documented from medical records.Since 3IC+3CCRT has been mostly administered in RCTs,the assessment of severity in this group might be more convincing than others.
Conclusions
This real-world analysis incorporated data from two epidemic centers and revealed that the 2IC+2CCRT modality was the optimal choice regarding efficacy,toxicity and cost-effectiveness for LA-NPC patients;however,2IC+2CCRT and 3IC+3CCRT probably shortened LRRFS in high-and low-risk populations,respectively.These findings could inform decision-making in clinical practice and the design of future RCTs.
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (No.81872375 and 82172863) and the Natural Science Foundation of Guangdong Province (No.2021A1515010118).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2023年2期
Chinese Journal of Cancer Research2023年2期
- Chinese Journal of Cancer Research的其它文章
- Stomach cancer burden in China: Epidemiology and prevention
- When immunotherapy meets liver transplantation for hepatocellular carcinoma: A bumpy but promising road
- Transforming cancer cells for long-term living with cancer:An inspiring new approach
- Variant rs8400 enhances ALKBH5 expression through disrupting miR-186 binding and promotes neuroblastoma progression
- Exploration and optimization of surgical techniques for laparoscopic transhiatal lower mediastinal lymph node dissection for adenocarcinoma of esophagogastric junction: A prospective IDEAL 2a study with qualitative design
- Aqueous-soluble components of sporoderm-removed Ganoderma lucidum spore powder promote ferroptosis in oral squamous cell carcinoma
