Propofol sedation in routine endoscopy: A case series comparing target controlled infusion vs manually controlled bolus concept
Riad Sarraj,Lorenz Theiler,Nima Vakilzadeh,Niklas Krupka,Reiner Wiest
Abstract BACKGROUND Many studies have addressed safety and effectiveness of non-anaesthesiologist propofol sedation (NAPS) for gastrointestinal (GI) endoscopy Target controlled infusion (TCI) is claimed to provide an optimal sedation regimen by avoiding under- or oversedation.AIM To assess safety and performance of propofol TCI sedation in comparison with nurse-administered bolus-sedation.METHODS Fouty-five patients undergoing endoscopy under TCI propofol sedation were prospectively included from November 2016 to May 2017 and compared to 87 patients retrospectively included that underwent endoscopy with NAPS. Patients were matched for age and endoscopic procedure. We recorded time of sedation and endoscopy,dosage of medication and adverse events.RESULTS There was a significant reduction in dose per time of propofol administered in the TCI group,compared to the NAPS group (8.2±2.7 mg/min vs 9.3±3.4 mg/min; P=0.046). The time needed to provide adequate sedation levels was slightly but significantly lower in the control group (5.3±2.7 min vs 7.7±3.3 min; P<0.001),nonetheless the total endoscopy time was similar in both groups. No differences between TCI and bolus-sedation was observed for mean total-dosage of propofol rate as well as adverse events.CONCLUSION This study indicates that sedation using TCI for GI endoscopy reduces the dose of propofol necessary per minute of endoscopy. This may translate into less adverse events. However,further and randomized trials need to confirm this trend.
Key Words: Sedation; Endoscopy; Propofol; Target controlled infusion; Non-anaesthesiologist propofol sedation; Adverse event
INTRODUCTION
Many studies have addressed the safety and effectiveness of non-anaesthesiologist propofol sedation (NAPS) for gastrointestinal (GI) endoscopy[1-5]. A high dose of propofol has been recognized as an independent risk factor for sedation-related complications[6]. For the safe use of propofol during endoscopic procedures performed by nonanaesthesiologists,controlled comparisons between different methods of propofol administration are still needed.
One of the most frequent methods of propofol sedation in GI endoscopy is manual administration of boluses. This method may be sub optimal during long-lasting endoscopies[7]. Target Controlled Infusion (TCI) is a delivery system with an infusion mode that uses pharmacokinetic models (based on age,sex,height,weight and dosing history in the individual patient) to calculate infusion rates required to reach and maintain a desired target concentration in the target tissue of the brain. Ultimately,the system is claimed to provide a calculated optimal sedation regimen hence avoiding under- or oversedation[8-10].
The aim of the present study was to assess safety and performance,in terms of time of sedation and dosage of propofol during TCI sedation in comparison with nurse-administered intermittent bolus propofol sedation.
MATERlALS AND METHODS
Study cohort
Forty-five consecutive patients undergoing endoscopy under TCI propofol sedation were prospectively included from November 2016 to Mai 2017. These were compared to a historic cohort of sex and age-matched patients that underwent endoscopy with bolus-sedation (n=80). These comparator patients were matched for type endoscopic procedure. Exclusion criteria were age under 18 years; pregnant and lactating women; American Society of Anaesthesiologists class IV; allergy to propofol,fentanyl,or benzodiazepine; and anticipated difficult airway.
Endoscopic procedures
Hospital faculty experienced endoscopists performed all endoscopic procedures in Table 1. Physical monitoring included heart rate,peripheral arterial oxygen saturation,and non-invasive blood pressure being monitored and recorded continuously with a bedside monitor. Blood pressure was recorded every 2 min. All patients received oxygen 2 L/minvianasal cannula throughout the procedure.
Drug administration and endpoint evaluation
Propofol was administered intravenously by using the Module Dependable Process Station TCI system (Fresenius Kabi,Bad Homburg,German) using the pharmacokinetic parameter set according to the Schnider model. The initial setting of the target blood concentration of propofol was set at 2.0 mg/mL. The predicted brain tissue concentration of propofol ateach time point was calculated automatically and was shown on the monitor of the TCI pump. The primary plasma target concentration was set at 1.5 g/mL with the possibility to increase the target by 0.3 g/mL every two minutes to a maximum of 3.5 g/mL. this adjustment was made upon the patients response based on the Observers Assessment of Alertness/Sedation (OAA/S) score[11].
Historic comparator sedation protocol: Manual sedation was following the "20/2 rule"[12] with an induction bolus dose of 0.5-1.0 mg/kg of propofol (Disoprivan 1%) followed by titration of maximum 20 mg every 2 min. Low doses of fentanyl bolus (25-100 g) could be added at the discretion of the endoscopist in both sedation regimens.
Once patient lost verbal command and eyelash reflex (OAA/S scores < 2) endoscopy was started. The induction period was defined as the time from the start of propofol infusion to insertion of the endoscope. The procedure time was defined as the time of the first endoscope insertion until endoscope removal.
Adverse events
Adverse events were defined as hypoxemia (peripheral oxygen saturation less than 90 %),hypotension (drop of mean arterial pressure below 60 mmHg),bradycardia (drop heart rate below 50 beats per minute for more than 1 min),and tachycardia (rise of heart rate above 110 beats per minute for more than 1 min). If hypoxemia occurred during the sedation,we performed chin lift on the patient and increased the oxygen dose.
Primary endpoint
The primary endpoint of the study was the consumption of propofol (mg) during endoscopy evaluated as dose (mg) per time (min).
Secondary endpoints include time of induction,total sedation time and safety regarding adverse events during sedation. The primary hypothesis stated that the use of TCI sedation would decrease the use of propofol over time and therefore be associated with a safer sedation.
Statistical analyses
All statistical analyses were performed with Stata 12.0. Results are presented as mean ± (SD). Differences between groups were calculated with Student’st-test,Wilcoxon rank sum test and Chi2test whenever appropriate. A value ofP<0.05 was regarded as significant.
RESULTS
All patients successfully underwent smooth procedures and no severe adverse event occurred. The demographic characteristics of the study participants did not show significant differences between the TCI group and the control group with respect to sex (female: 57%vs43%;P=0.67) and median age (55.9vs56.2;P=0.17).
Endoscopy characteristics are shown in Table 1 and did not differ significantly between groups (P=0.55).
The average total propofol consumption did not significantly differ between the groups (378.6±213.1 mgvs340.07±150.07 mg;P=0.59). However,there was a significant reduction in dose per time of propofol administered in the TCI group,compared to the bolus group (8.2±2.7 mg/minvs9.3±3.4 mg/min;P=0.046,Figure 1).
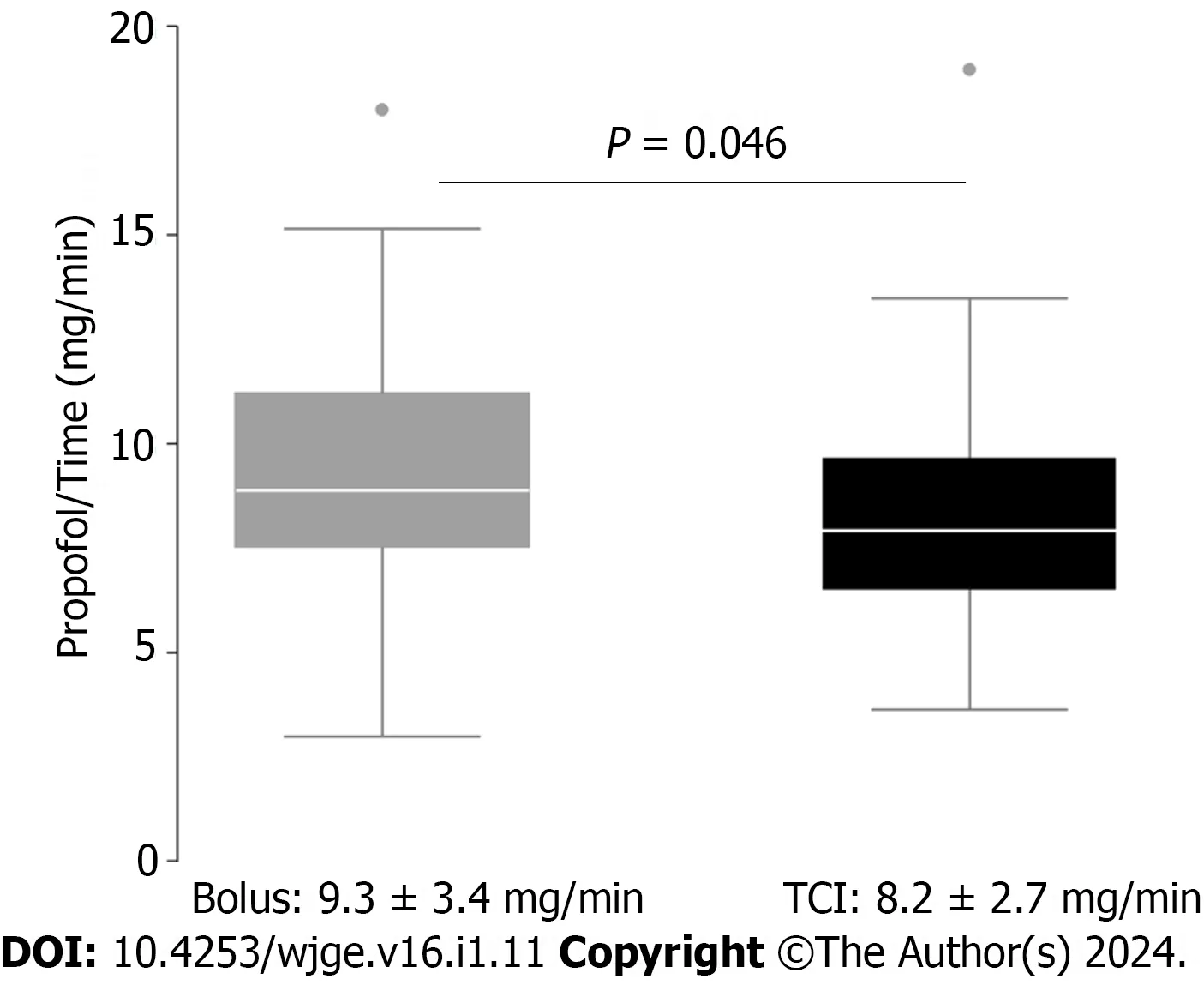
Figure 1 Propofol dose/time (mg/min). TCI: Target controlled infusion.
The time needed to provide proper sedation level was slightly but statistically significantly lower in the control group (5.3±2.7 minvs7.7±3.3 min;P<0.01). Nonetheless,the total endoscopy time was not different (42.3±19.3 minvs43.5±18.2 min;P=0.57).
There were no significant differences in the number of interventions utilizing fentanyl (71.2%vs73.3%P=0.8). However,average dose of fentanyl being used was significantly less in the TCI as compared to the control group (59.14±28.37ugvs36.67±16.52 g;P0.01).
No difference between bolus-sedation and TCI was observed for the rate of adverse events (26%vs24%;P=0.95,Table 2).

Table 2 Number and percentage of adverse events [n (%)]
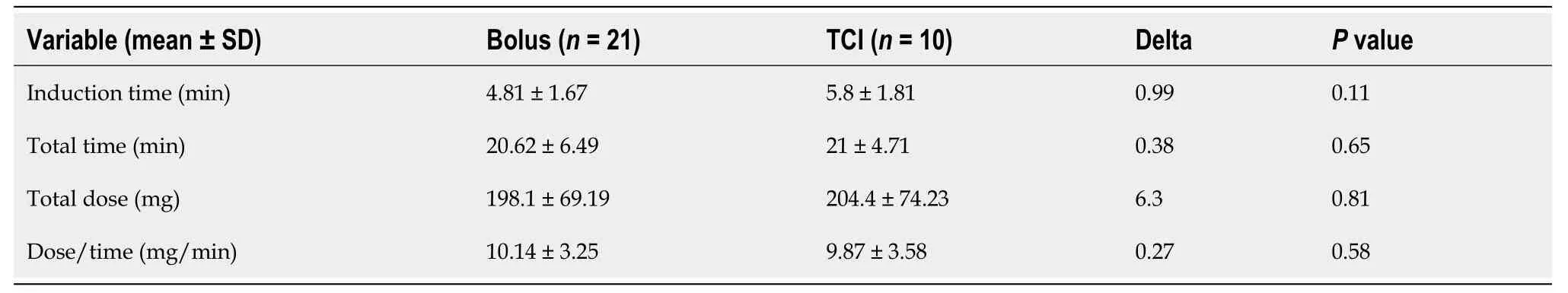
Table 3 Subgroup analysis according to duration of endoscopy: Short endoscopy < 30 min
We ran a subgroup analysis with either short (less than 30 min) or long (more than 1 h) exams,for which results are shown in Tables 3 and 4. We found no significant reduction of dosage per time in favour of the TCI group looking at longer exams (8.94±3.21 mg/minvs6.82±2.44 mg/min;P=0.08,Figure 2). A reduction in total propofol dose in favourof the TCI group was observed looking at longer exams; this did not reach statistical significance (656.15±291.42vs484.67±200.02;P=0.27).
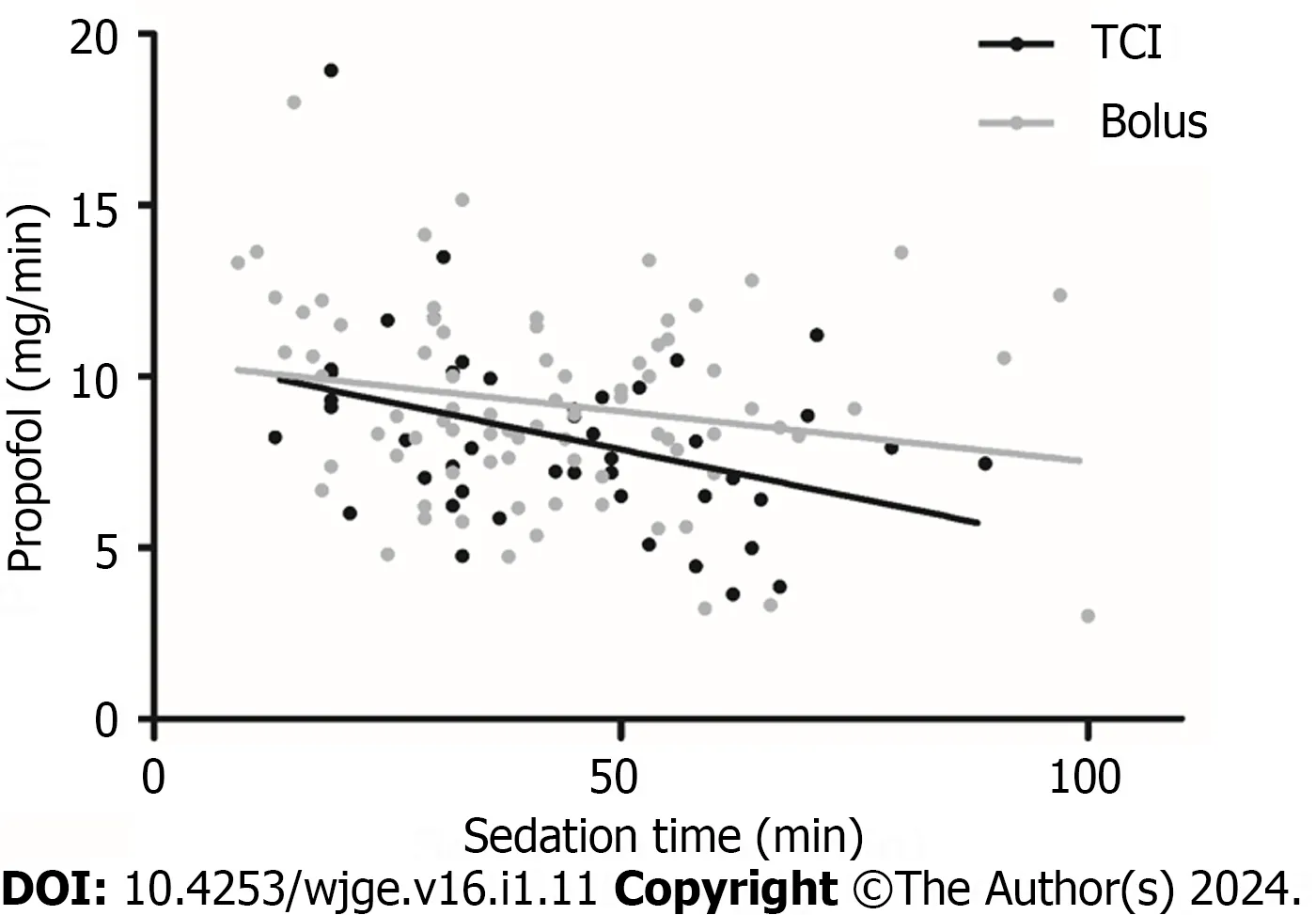
Figure 2 Propofol dose/time (mg/min) over sedation time.TCI: Target controlled infusion.
DlSCUSSlON
Propofol has been widely accepted as an ideal agent for endoscopy sedation because of the rapid onset of action and short recovery time[1,2]. However,propofol may cause cardiorespiratory inhibition necessitating providing of cardiorespiratory support with a ventilator until propofol is metabolized because there are no antagonists available. Thus,it is necessary to keep a balance between adequate sedation depth and minimized adverse effects. Intermittent bolus and continuous infusion are both alternatives for administration of propofol. However,the great variation in individual responses to propofol may be an important concern regarding safety during endoscopies[13].
During time-consuming endoscopic procedures,it may be difficult to obtain the optimal titration of drugs without increasing the risks of severe hypoxia,prolonged sedation and patient discharge after procedure[14].
Among different systems available for propofol administration,TCI uses a pharmacokinetic model to achieve and maintain a selected target plasma propofol concentration,through variation of the infusion rate,with a good predictive performance[8]. Previous studies on the use of TCI-based propofol administration demonstrated its feasibility and help in avoiding over- or under-sedation GI endoscopy[9,10]. Specifically,TCI-administered propofol sedation has been reported to achieve higher endoscopists satisfaction score,faster recovery of patients and more stable hemodynamic and respiratory conditions during endoscopy than manual infusion regimens particularly in hands of unexperienced training anaesthesiologists[15-17].
TCI-based propofol sedation has been evaluated in large series of various endoscopic procedures demonstrating safety and benefits[18,19].
The results of our study indicate that sedation using TCI for GI endoscopy reduces the dose of propofol necessary per minute of endoscopy. All procedures were carried out successfully and both methods of sedation were associated with adequate clinical sedation levels.
The occurrence of adverse events (around 25% in both groups) may seem high. However,we used very sensitive and conservative cut-offs to define adverse events,most of which were not severe or even life threatening. It is important to emphasie that our cohort didn’t include any patients who would have increased risk for and/or require per se a higher dosage of propofol known as confounding factors such as: Primary Sclerosing Cholangitis,IV Drug users,bad experience in pervious endoscopy,patients with severe pain syndromes and/or being on opiates.
We also ran a subgroup analysis with either short (less than 30 min) or long (more than 1 h) exams,expecting to find better results with longer endoscopy procedure.
The analysis is therefore based on fewer results and the results did not reach statistical significance,but we found a trend tend towards reduction of dosage per time (2.12 mg/min) in favour of the TCI group. It may also be interesting to note that a reduction of total propofol dose of approximatively 170 mg in favour of the TCI group was found,even if this difference did not reach statistical significance because of the large variance.
Another advantage that was stated by the nursing staff is the convenience of the pump,allowing for more time and focus for the endoscopy nurse to help with the procedure if necessary,as well as the fewer manual interactions of the syringes,which reduces the risk of contamination.
Interestingly,significantly less fentanyl was used in the TCI group. This could be interpreted as a relative underuse of propofol in the bolus group,where the total amount of propofol would have been expected to be higher compared to the TCI group. It seemed that in the bolus group,at least some of the propofol was substituted by fentanyl.
CONCLUSION
In conclusion,our study indicates that sedation using TCI for GI endoscopy reduces the dose of propofol necessary per minute of endoscopy and this could have an impact especially on prolonged endoscopy procedures. This may also translate into less adverse events and higher safety when using TCI in prolonged procedures. However,further studies on large scale with prospective randomized-controlled design are needed to standardize sedation with propofol. With proper education,TCI sedation could then be implemented in routine endoscopy procedures.
ARTlCLE HlGHLlGHTS
Research background
Non-anaesthesiologist propofol sedation (NAPS) for gastrointestinal (GI) endoscopy is safe and effective. Target controlled infusion (TCI) is claimed to provide an optimal sedation regimen by avoiding under or over-sedation.
Research motivation
Little is known about the differences of time of sedation and propofol dosage between nurse-administered intermittent bolus propofol sedation and TCI.
Research objectives
The aim of this study is to assess safety and performance of propofol TCI sedation in comparison with nurseadministered bolus-sedation.
Research methods
Forty-five patients undergoing endoscopy under TCI propofol sedation were prospectively included from November 2016 to May 2017 and compared to 87 patients retrospectively included that underwent endoscopy with NAPS.
Research results
Sedation using TCI for GI endoscopy reduces the dose of propofol necessary per minute of endoscopy (8.2±2.7 mg/minvs9.3±3.4 mg/min;P=0.046). Time needed to provide adequate sedation levels was lower in the control group. No differences between TCI and bolus-sedation was observed for mean total-dosage of propofol rate as well as adverse events.
Research conclusions
Sedation using TCI for GI endoscopy reduces the dose of propofol necessary per minute of endoscopy.
Research perspectives
Sedation using TCI for GI endoscopy could have an impact on propofol total dosage especially on prolonged endoscopy procedures. This may also translate into less adverse events and higher safety when using TCI in prolonged procedures.
FOOTNOTES
Author contributions:Sarraj R collected the dataset,wrote and designed the manuscript and figures; Vakilzadeh N provided support for the statistical analysis and figure design; Krupka N reviewed the manuscript and supported the submission; Theiler L and Wiest R designed the trial and implemented the TCI use in clinical practice and reviewed and the manuscript.
lnstitutional review board statement:The study was reviewed and approved by the Gesundheits-,Sozial-und Integrations direktion Kantonale Ethikkommission für die Forschung.
Conflict-of-interest statement:No conflict-of-internest to disclose.
Data sharing statement:Technical appendix,statistical code,and dataset available from the corresponding author at riad.sarraj@insel.ch. patient consent was not obtained but the presented data are anonymized and risk of identification is low.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Switzerland
ORClD number:Riad Sarraj 0000-0003-4710-3704; Reiner Wiest 0000-0002-1469-7107.
S-Editor:Lin C
L-Editor:A
P-Editor:Cai YX
 World Journal of Gastrointestinal Endoscopy2024年1期
World Journal of Gastrointestinal Endoscopy2024年1期
- World Journal of Gastrointestinal Endoscopy的其它文章
- Bowel preparation protocol for hospitalized patients ages 50 years or older: A randomized controlled trial
- Safety and efficacy of modified endoscopic ultrasound-guided selective N-butyl-2-cyanoacrylate injections for gastric variceal hemorrhage in left-sided portal hypertension
- Adverse events associated with the gold probe and the injection gold probe devices used for endoscopic hemostasis: A MAUDE database analysis
- Upper gastrointestinal bleeding in Bangladeshi children: Analysis of 100 cases
