Safety and efficacy of modified endoscopic ultrasound-guided selective N-butyl-2-cyanoacrylate injections for gastric variceal hemorrhage in left-sided portal hypertension
Yan Zeng,Jian Yang,Jun-Wen Zhang
Abstract BACKGROUND Gastric variceal hemorrhage is one of the primary manifestations of left-sided portal hypertension (LSPH). The hemorrhage is fatal and requires safe and effective interventions.AIM To evaluate the clinical safety and efficacy of modified endoscopic ultrasound (EUS)-guided selective N-butyl-2-cyanoacrylate (NBC) injections for gastric variceal hemorrhage in LSPH.METHODS A retrospective observational study of patients with LSPH-induced gastric variceal hemorrhage was conducted. Preoperative EUS evaluations were performed. Enrolled patients were divided into modified and conventional groups according to the NBC injection technique. The final selection of NBC injection technique depended on the patients’ preferences and clinical status. The technical and clinical success rates,operation time,NBC doses,perioperative complications,postoperative hospital stay,and recurrent bleeding rates were analyzed,respectively.RESULTS A total of 27 patients were enrolled. No statistically significant differences were observed between the two groups regarding baseline characteristics. In comparison to patients in the conventional group,patients in the modified group demonstrated significantly reduced NBC doses (2.0±0.6 mL vs 3.1±1.0 mL; P=0.004) and increased endoscopic operation time (71.9±11.9 min vs 22.5±6.7 min; P<0.001). Meanwhile,the two groups had no significant difference in the technical and clinical success rates,perioperative complications,postoperative hospital stay,and recurrent bleeding rates.CONCLUSION Modified EUS-guided selective NBC injections demonstrated safety and efficacy for LSPH-induced gastric variceal hemorrhage,with advantages of reduced injection dose and no radiation risk. Drawbacks were time consumption and technical challenge.
Key Words: Endoscopic ultrasound; Selective; N-butyl-2-cyanoacrylate; Gastric varices; Hemorrhage; Left-sided portal hypertension
INTRODUCTION
Left-sided portal hypertension (LSPH) is caused by splenic vein stenosis,thrombosis,or obstruction,with pancreatic diseases as the most common etiology[1,2],among which pancreatitis and pancreatic tumors account for the leading causes of LSPH[3,4]. Clinical symptoms of LSPH are attributed to an increase in the pressure gradient between the portal vein and the inferior vena cava[5]. Gastric variceal hemorrhage is one of the primary manifestations and the foremost cause of emergency department visits in LSPH patients[6],first described in 1969[7]. Given normal liver function and no obvious clinical symptoms in LSPH patients,gastric varices (GV) have received little attention,and their hemorrhage can be unexpected and fatal[8]. Thus,safe and effective interventions are required.
In recent years,the widespread use of digestive endoscopy in clinical practice has led to a gradual shift in patient preference towards minimally invasive endoscopic techniques,especially in the field of endoscopic ultrasound (EUS)[9,10]. EUS has demonstrated convenience and promise in diagnostic procedures and hemostatic interventions for GV due to the combined function of endoscopy and ultrasound[11]. Moreover,EUS-guided GV therapy offers a safer and more practical alternative than the conventional therapy of endoscopic N-butyl-2-cyanoacrylate (NBC) injection[12,13].
Based on previous studies,we reported a modified EUS-guided selective NBC injection procedure in a patient with LSPH-induced gastric variceal hemorrhage[6]. The preliminary advantages of this modified procedure included reduced NBC doses,radiation avoidance,and a firmer obliteration effect with fewer rebleedings caused by glue ulcers[6]. We conducted this retrospective study in our single center to verify these clinical values and provide more basis for future research on EUS-guided GV treatment.
MATERlALS AND METHODS
Study design and study population
This retrospective study received approval from the Ethics Committee of The First Affiliated Hospital of Chongqing Medical University. We retrospectively reviewed qualified LSPH patients from the First Affiliated Hospital of Chongqing Medical University from October 2019 to September 2023. All enrolled patients were diagnosed with LSPH-induced gastric variceal hemorrhage and received endoscopic NBC injections. Written informed consent was obtained from all the patients before each endoscopic procedure. Exclusion criteria included previous endoscopic hemostasis,severe organ dysfunction,or other conditions unsuitable for endoscopic procedures.
Endoscopic interventions
The final selection of NBC injection technique types (modified EUS-guided selective NBC injection or conventional endoscopic NBC injection) depended on the patients’ preferences and clinical status. Patients electing conventional endoscopic NBC injection constituted the conventional group and received conventional sandwich injection[14],while patients electing modified EUS-guided selective NBC injection formed the modified group and received selective NBC injection under EUS guidance (Linear Pentax echoendoscope,Hoya Co.,Tokyo,Japan) (Figure 1)[6].
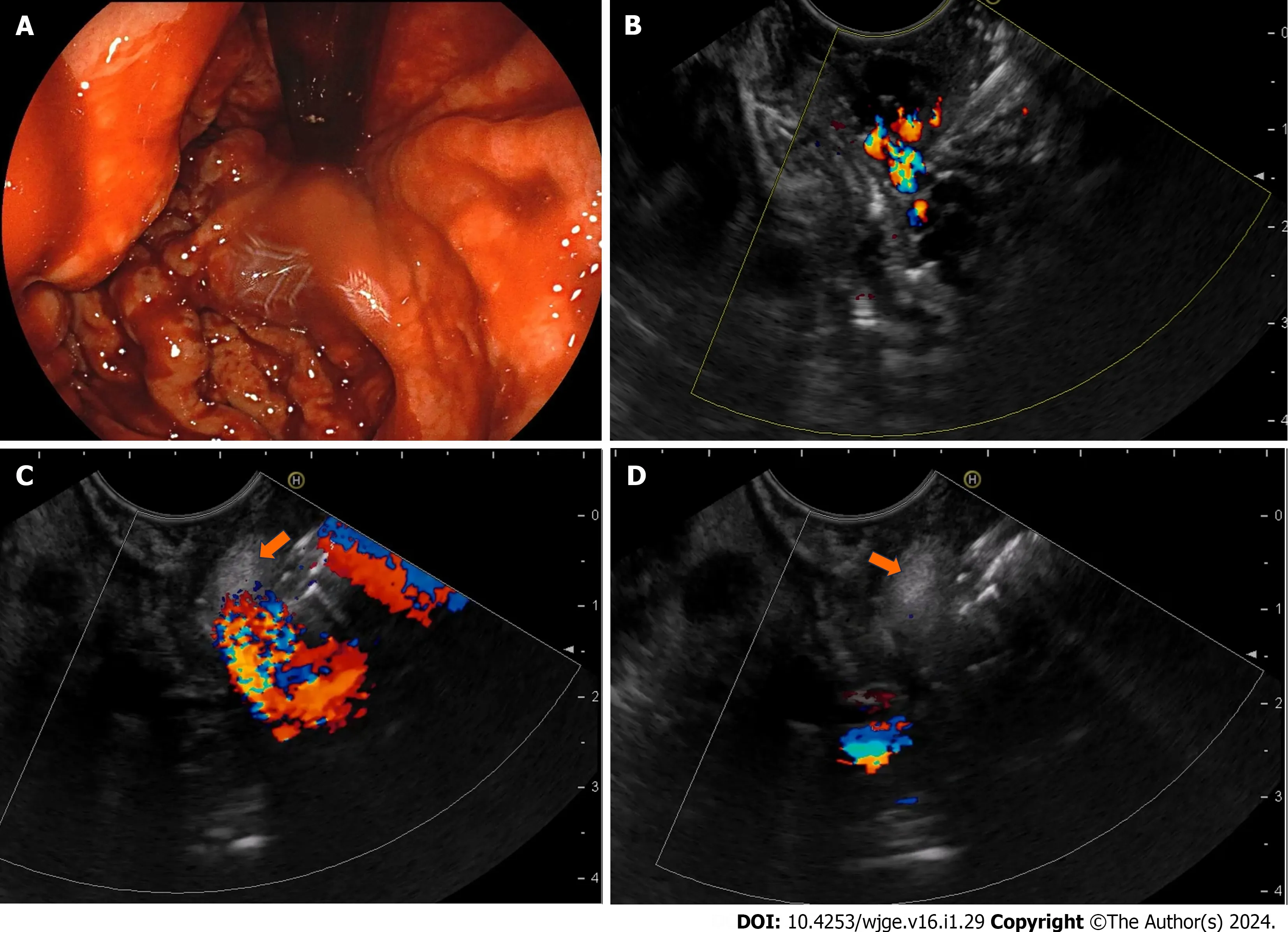
Figure 1 Endoscopic procedure for patients in modified group. A: Gastroscopy revealed gastric varices (GV) with active bleeding;B: A confluence of GV was identified and selected as the injection site;C: N-butyl-2-cyanoacrylate (orange arrow) was injected into the selected gastric varix;D: Hyperechoic fillings (orange arrow) and decreased blood flow signals were observed after injections.
Postoperative follow-up and data collection
The technical and clinical success rates,operation time,NBC doses,perioperative complications,and postoperative hospital stay were collected from inpatient medical records and analyzed. The follow-up records were reviewed 1,3 and 6 mo after the NBC injections. Recurrent upper gastrointestinal hemorrhage rates were derived from the routine outpatient follow-up at the Gastroenterology Department. Only patients with complete medical records were included.
Data analysis
Continuous variables and categorical were expressed as means ± SD andn(%),respectively. Unpaired Student’sttest and Mann-WhitneyUtest were used for continuous variables,while theχ2and Fisher’s exact tests were performed for categorical variables. Statistical analyses were performed using SPSS 23.0,and statistical significance was defined asP<0.05.
RESULTS
Patient characteristics
This study preliminarily enrolled 30 patients. However,some participants underwent splenectomy or had both modified EUS-guided selective NBC injection procedures and conventional endoscopic NBC injection procedures during the follow-up period and,therefore,were excluded. Thus,the final number of qualified participants in the conventional and modified groups was 16 and 11,respectively (Figure 2). Significant differences were not observed between the two groups regarding baseline characteristics (Table 1). The median age was 46.6 (range 24.0-68.0) years for the modified group and 47.9 (range 29.0-68.0) years for the conventional group. Seven patients in the modified group (63.6%) and 11 in the conventional group (68.8%) were male (P=0.78). In all enrolled patients,the three most common causes for LSPHinduced GV hemorrhage were,in order,walled-off necrosis (12/27,44.4%),pancreatic pseudocyst (8/27,29.6%) and pancreatitis (5/27,18.5%). Eight patients in the modified group (72.8%) and 12 in the conventional group (75.0%) were diagnosed with walled-off necrosis or pancreatic pseudocyst (P=0.93) (Table 1).
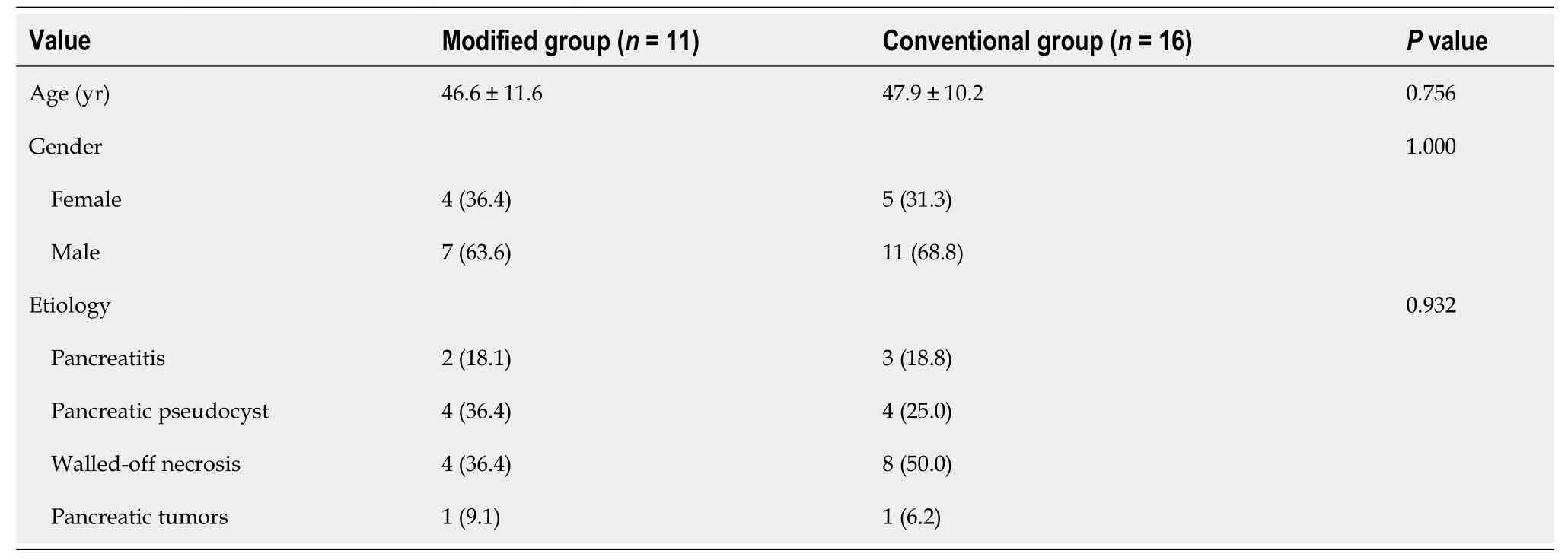
Table 1 Study population and comparison of two groups,n (%)
Safety and efficacy of endoscopic procedures in two groups
Technical success was defined as successful injection and absolute occlusion of the targeted GV,while clinical success was defined as the resolution or improvement of gastric variceal hemorrhage. The technical success rate was 100% for both types of injection procedures,and clinical success rates were 90.9% and 100% in the modified and conventional groups,respectively (P=0.41). The technical and clinical success rates were not significantly different between the groups (Table 2).
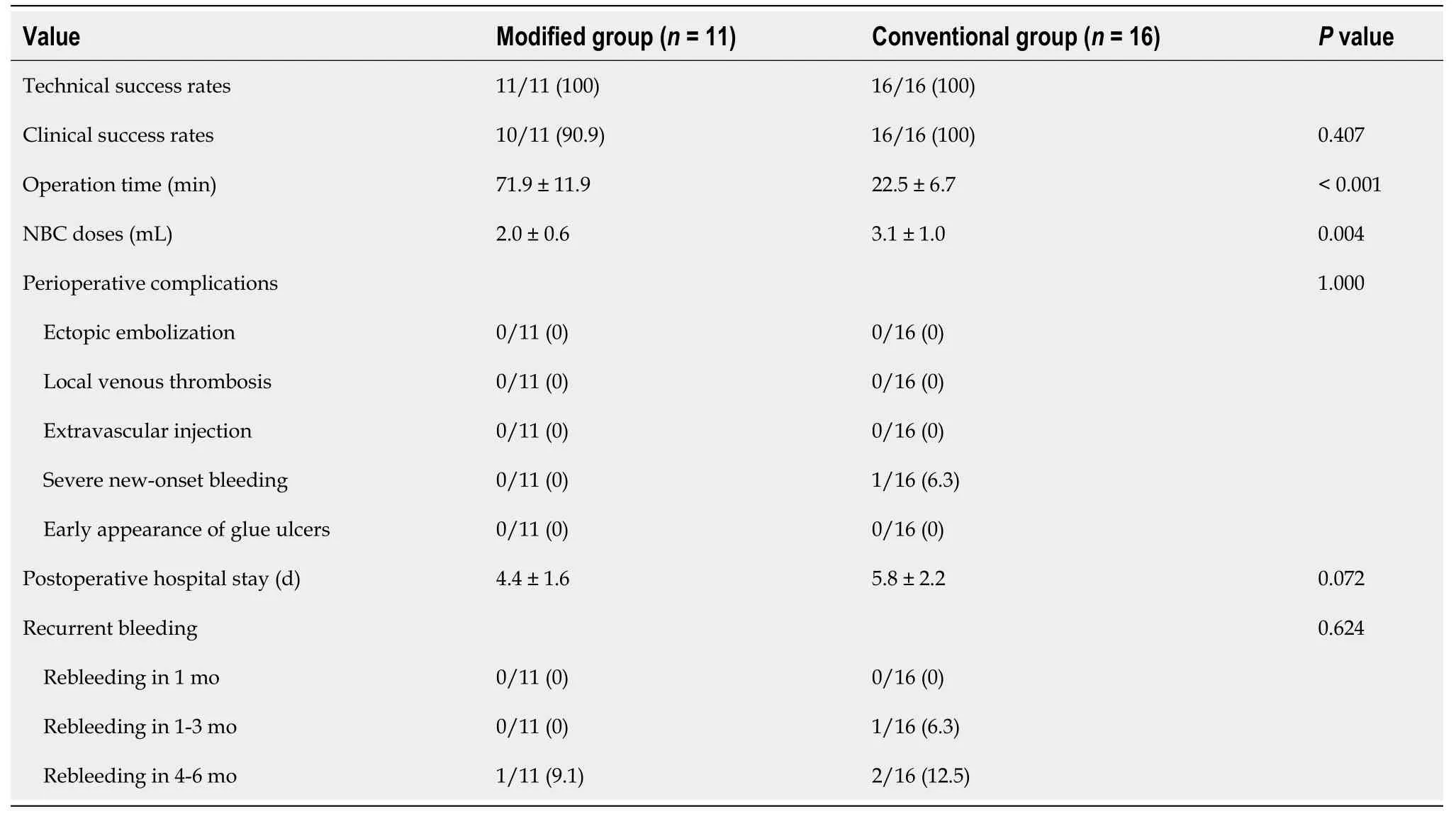
Table 2 Endoscopic operation and follow-up data of two groups,n (%)
Perioperative complications included ectopic embolization,local venous thrombosis,extravascular injection,severe new-onset bleeding following the needle removal,and the early appearance of glue ulcers[15,16]. In comparison to patients in the conventional group,patients in the modified group demonstrated significantly reduced NBC doses (2.0±0.6 mLvs3.1±1.0 mL;P=0.004) and increased endoscopic operation time (71.9±11.9 minvs22.5±6.7 min;P<0.001). Meanwhile,the perioperative complications,postoperative hospital stay,and recurrent bleeding rates for patients in the modified group were 0%,4.4±1.6 d,and 9.1%,respectively,vs6.3%,5.8±2.2 d,and 18.8% for those in the conventional group. The two groups had no significant difference in the perioperative complications,postoperative hospital stay,and recurrent bleeding rates (Table 2).
DlSCUSSlON
This present study built on our prior research and compared the safety and efficacy of a modified EUS-guided selective NBC injection procedure for gastric variceal hemorrhage in LSPH with conventional endoscopic NBC injection procedures. To the best of our knowledge,no similar studies had previously been reported in the literature.
Our result revealed consistency with previous research that LSPH was most common in patients with pancreatic disease,especially those with walled-off necrosis and pancreatic pseudocyst[17,18],which occurred because of the anatomical proximity between the splenic vein and the pancreas[6]. Therefore,regular follow-ups should be scheduled for LSPH patients to reduce unexpected and fatal bleeding. Moreover,when considering endoscopic minimally invasive procedures,sufficient attention to intraoperative and postoperative bleeding should be paid to patients with pancreatic pseudocysts or walled-off necrosis[2,19].
Although endoscopic NBC injection was recommended with great clinical value in achieving hemostasis in LSPH patients[20],conventional injection procedures have striking defects in identifying varices below the gastric mucosal layer,locating culprit vessels during massive gastric hemorrhage,and reducing possible operation-related complications,including ectopic embolization and extravascular injection[21-23]. These deficiencies also place new demands on further developments of endoscopic procedures. EUS is a productive and promising approach to perform real-time ultrasonic scanning and interventions for GV,perforating feeding veins,portal vein and its tributaries,and collateral circulation[11,24]. EUS-guided NBC injection in GV patients revealed superior clinical outcomes than conventional endoscopic injection dual to properties of NBC dosage reduction,better obliteration,and fewer recurrences and rebleedings[13,25].
We applied this modified EUS-guided selective NBC injection in LSPH-induced gastric variceal hemorrhage patients,and we found that it was,first and foremost,safe and effective in this retrospective study in our single center. Safety is the primary premise and final goal of exploring technical development. Compared with conventional endoscopic injection,this modified procedure did not increase the incidence of perioperative complications,nor would it prolong the patient's hospital stay. Meanwhile,more cases were included in this study to verify our previous research and testify to the benefits of NBC dosage reduction and its consequent reduced medical cost and complications[6]. Reducing gluerelated complications focuses on effectively minimizing the injection dose,including endoscopic clips-assisted injection,balloon-occluded retrograde transvenous obliteration (BRTO),combined deployment of embolization coils and cyanoacrylate,and our modified procedure[26-28]. Each of these above procedures has its own advantages and applicable population. The modified procedure in our study can locate the puncture site more accurately in real time; the injection depth and angle can be precisely controlled; the injection can be timely terminated through observing the real-time flow blocking effect; and it can help avoid extravascular injection and reduce the total injection dose; avoid radiation exposure during the combined coil deployment or BRTO; and reduce related medical costs. It is also worth noting that the operation time was significantly longer in the modified group than in the conventional group. We considered that was relevant to time consumption in confirming the ideal puncture site during the EUS procedure. Therefore,this method is currently unsuitable for endoscopic centers lacking relevant experience,nor is it applicable for critically ill patients with unstable vital signs who need urgent endoscopic hemostasis.
EUS technology and equipment have not been satisfactorily popularized in many Asian regions,and there is still a significant training demand for many endoscopic interventional operations,including EUS-guided GV procedures[29]. Compared to these more difficult and time-consuming EUS-guided GV procedures,the technique and equipment required for conventional injection are more accessible to acquire and,therefore,cannot be discarded[30]. It was also noticed in the inclusion phase of this study that two patients shifted from the original modified procedure to the conventional method in their follow-up endoscopic treatment. We presume that this was because of the advantages of the conventional operation in reducing difficulties and operation time. Consequently,a multidisciplinary discussion team is a widely recommended approach to selecting the most appropriate individual treatment.
There were three main limitations. First,this was a retrospective observational study. Our findings are limited by the study design,and future prospective randomized controlled studies are needed. Second,this was a single-center study,and EUS-guided operations are noticeably affected by technical conditions and experience levels. In the future,multicenter studies involving more endoscopy centers in multiple tertiary hospitals are needed. Third,the sample size was small and had a specific regional characteristic. On the one hand,the small number of enrolled patients was because LSPH is a rare cause of GV and consequent hemorrhage[31,32]. On the other hand,since the our endoscopic center is a regional center for treating severe pancreatitis,most patients included in this study had complications such as pancreatic pseudocyst or walled-off necrosis,which may have had an unavoidable impact on the results. Therefore,future studies need to include more LSPH patients with varied causes.
CONCLUSION
Modified EUS-guided selective NBC injections demonstrated safety and efficacy for LSPH-induced gastric variceal hemorrhage,with advantages mainly in reducing injection dose and having no radiation risk. The drawbacks included that the procedure was time-consuming and technically challenging to perform. Therefore,this procedure is recommended for complicated patients in experienced endoscopy centers.
ARTlCLE HlGHLlGHTS
Research background
Left-sided portal hypertension (LSPH) is often secondary to pancreatic diseases,including pancreatitis and pancreatic tumors. Given normal liver function and no obvious clinical symptoms in LSPH patients,gastric varices (GV) have received little attention.
Research motivation
To study the clinical value of our previously reported modified endoscopic ultrasound (EUS)-guided selective N-butyl-2-cyanoacrylate (NBC) injection procedure in patients with LSPH-induced gastric variceal hemorrhage.
Research objectives
To evaluate and compare the clinical safety and efficacy between modified EUS-guided selective NBC injections and conventional endoscopic NBC injection procedures for gastric variceal hemorrhage in LSPH.
Research methods
LSPH patients from the First Affiliated Hospital of Chongqing Medical University were retrospectively reviewed and analyzed from October 2019 to September 2023. The technical and clinical success rates,operation time,NBC doses,perioperative complications,postoperative hospital stay,and recurrent bleeding rates of the modified and conventional groups were analyzed.
Research results
The technical success rate was 100% for both types of injection procedures,and clinical success rates were 90.9% and 100% in the modified and conventional groups,respectively (P=0.41). In comparison to patients in the conventional group,patients in the modified group demonstrated significantly reduced NBC doses (2.0±0.6 mLvs3.1±1.0 mL;P=0.004) and increased endoscopic operation time (71.9±11.9 minvs22.5±6.7 min;P<0.001). Meanwhile,the perioperative complications,postoperative hospital stay,and recurrent bleeding rates for patients in the modified group were 0%,4.4±1.6 d,and 9.1%,respectively,vs6.3%,5.8±2.2 d,and 18.8% for those in the conventional group.
Research conclusions
The modified EUS-guided selective NBC injection procedure demonstrated reduced injection dose and no increased perioperative complications compared to conventional endoscopic NBC injection procedures. Thus,it is safe and effective in treating patients with LSPH-induced gastric variceal hemorrhage.
Research perspectives
This present study built on our prior research and compared the safety and efficacy of a modified EUS-guided selective NBC injection procedure for gastric variceal hemorrhage in LSPH with conventional endoscopic NBC injection procedures. EUS-guided advanced endoscopic procedures will undoubtedly be the future direction of endoscopic treatment.
FOOTNOTES
Author contributions:Zeng Y,Yang J and Zhang JW conceptualized and designed the research; Zeng Y and Yang J performed the literature search,analyzed the data,and wrote the original manuscript; Yang J and Zhang JW performed the endoscopic procedures and edited the final manuscript; all authors have read and approved the final manuscript.
Supported byProgram for Youth Innovation in Future Medicine,Chongqing Medical University,China,No. W0138.
lnstitutional review board statement:This retrospective study received approval from the Ethics Committee of The First Affiliated Hospital of Chongqing Medical University.
lnformed consent statement:All study participants,or their legal guardian,provided informed written consent prior to study enrollment.
Conflict-of-interest statement:The authors declare that they have no competing interests.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement-checklist of items,and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yan Zeng 0000-0003-4935-1306; Jian Yang 0000-0001-8170-0727; Jun-Wen Zhang 0000-0003-2911-598X.
Corresponding Author's Membership in Professional Societies:Digestive Endoscopy Branch of Chinese Medical Association.
S-Editor:Gao CC
L-Editor:Kerr C
P-Editor:Cai YX
 World Journal of Gastrointestinal Endoscopy2024年1期
World Journal of Gastrointestinal Endoscopy2024年1期
- World Journal of Gastrointestinal Endoscopy的其它文章
- Propofol sedation in routine endoscopy: A case series comparing target controlled infusion vs manually controlled bolus concept
- Bowel preparation protocol for hospitalized patients ages 50 years or older: A randomized controlled trial
- Adverse events associated with the gold probe and the injection gold probe devices used for endoscopic hemostasis: A MAUDE database analysis
- Upper gastrointestinal bleeding in Bangladeshi children: Analysis of 100 cases
