经鼻高流量氧疗与常规氧疗在急诊科心源性肺水肿应用的对比研究
杨志扬 黄志俭 吴爱群 陈轶强 周红 孙斐予
【摘要】 目的:探讨经鼻高流量氧疗(HFNC)对心源性肺水肿(ACPE)的临床应用价值。方法:选取本院收治的ACPE患者29例,根据方法不同,将其分为常规氧疗组(A组)13例和HFNC治疗组(B组)16例。比较两组治疗前后的临床指标(Borg评分、HR、MAP、PaO2、PaCO2、SaO2、pH值、RR)、症状缓解时间、有创通气率、病死率及疗效。结果:治疗半小时后,B组HR、RR、Borg评分均低于A组,PaO2、SaO2水平均高于A组,差异均有统计学意义(P<0.05),但两组MAP、pH、PaCO2水平比较,差异均无统计学意义(P>0.05);B组症状缓解时间短于A组(P<0.05);两组有创通气率、病死率、有效率比较,差异均无统计学意义(P>0.05)。结论:HFNC能快速改善ACPE患者的临床指标,缓解呼吸困难症状,故HFNC可能是治疗ACPE的有效辅助手段。
【关键词】 经鼻高流量氧疗; 心源性肺水肿; 常规氧疗
【Abstract】 Objective:To explore the clinical application value of high flow nasal cannulae therapy(HFNC)in acute cardiogenic pulmonary edema(ACPE).Method:A total of 29 patients with ACPE admitted to our hospital were selected,according to different methods,they were divided into 13 cases of conventional oxygen therapy group(A group)and 16 cases of HFNC treatment group(B group).The clinical indicators(Borg score,HR,MAP,PaO2,PaCO2,SaO2,pH value,RR)before and after treatment,symptom relief time,invasive ventilation rate,mortality rate and curative effect between two groups were compared.Result:After half an hour of treatment,the HR,RR and Borg scores in B group were lower than those of A group,the PaO2 and SaO2 levels were higher than those of A group,the differences were statistically significant(P<0.05),but the levels of MAP,pH and PaCO2 in two groups were compared,the differences were not statistically significant(P>0.05).The remission time of symptoms in B group was shorter than that of A group(P<0.05),the invasive ventilation rate,mortality rate and effective rate in two groups were compared,the differences were not statistically significant(P>0.05).Conclusion:HFNC can rapidly improve the clinical indicators of ACPE patients and relieve dyspnea symptoms,so HFNC may be an effective adjuvant therapy for ACPE.
【Key words】 High flow nasal cannulae therapy; Cardiogenic pulmonary edema; Conventional oxygen therapy
First-authors address:Xiamen Traditional Chinese Medicine Hospital Affiliated to Beijing University of Traditional Chinese Medicine,Xiamen 361009,China
doi:10.3969/j.issn.1674-4985.2019.10.031
急性心源性肺水腫(acute cardiogenic pulmonary edema,ACPE)是内科较为常见的急危重症之一,常伴随严重低氧血症,病死率高达10%~20%[1-2]。对于此类疾病的救治,急诊科往往是首当其冲,快速有效的缓解患者症状十分重要。近年来,一种新型的无创通气方式-经鼻高流量氧疗(high flow nasal cannulae therapy,HFNC),对心肺有一定的支持功能,并且耐受性好、对气道有加温和湿化的优点,故而被认为是可替代或与无创正压通气(NIPPV)相媲美的呼吸治疗措施[3-5]。NIPPV对于ACPE有较明确的疗效,那么HFNC是否有效,目前相关研究报道较少。故本文选取本院急诊抢救室收治的ACPE患者,分别给予常规氧疗、HFNC治疗,以分析其应用价值,现报道如下。
1 资料与方法
1.1 一般资料 选取2017年2月-2018年3月本院收治的ACPE患者。(1)纳入标准:①符合ACPE诊断标准[6];②心功能Ⅳ级;③急查心电图和肌钙蛋白排除急性心肌梗死;④年龄>18岁。(2)排除标准:①严重心律失常、其他脏器功能衰竭、支气管哮喘和慢性阻塞性肺病者,有严重的神经系统损害和肺部感染者;②在抢救过程中死亡的患者;③血流动力学不稳定者(动脉收缩压<80 mm Hg);④严重心功能不全(EF<25%)或心跳、呼吸停止者;⑤意识障碍、自主呼吸微弱或停止者;⑥误吸危险性高、完全不能清除上呼吸道分泌物,痰液黏稠或气道分泌物过多,不能进行有效咳痰者;⑦休克、消化道穿孔/大出血,严重脑部疾病者;⑧未引流的血气胸、纵隔气肿者。最终纳入本研究29例,根据方法不同,将其分为常规氧疗组(A组)13例和HFNC治疗组(B组)16例。患者均已签署知情同意书,且本研究已经院伦理委员会审核批准。
1.2 方法 患者均给予镇静、强心、利尿、血管扩张药、纠正电解质紊乱和容量平衡、解痉、平喘治疗,A组给予常规氧疗,B组给予HFNC治疗。其中HFNC参数设置:应用费雪派克公司经鼻高流量吸氧仪器与鼻塞导管,初始设置为流量45 L/min,温度37 ℃,FiO2为100%,再依据氧合情况,逐步调高流量。治疗失败标准(气管插管指征):心脏或呼吸骤停需要心肺复苏;出现循环不稳定,如休克或严重心律失常;有呼吸肌疲劳表现的顽固渐进性的低氧血症(高流量面罩吸氧或无创通气PaO2<60 mm Hg)和重度高碳酸血症(PaCO2>90 mm Hg);出现昏迷。
1.3 观察指标及判定标准 (1)比较两组治疗前后的临床指标情况,包括呼吸困难(Borg)评分、心率(HR)、平均动脉压(MAP)、氧分压(PaO2)、二氧化碳分压(PaCO2)、氧饱和度(SaO2)、pH值、呼吸频率(RR)。(2)比较两组症状缓解时间、有创通气率、病死率及疗效。疗效评价标准。有效:呼吸困难、两肺哮鸣音和湿性啰音均消失或显著减轻,心率、呼吸频率、血压、PaO2、PaCO2、SaO2恢复正常或接近正常水平;无效:未达到有效标准,或有恶化倾向,需进一步治疗者。
1.4 统计学处理 使用SPSS 17.0软件对所得数据进行统计分析,计量资料用(x±s)表示,组间比较采用t检验;计数资料以率(%)表示,比较采用字2检验。以P<0.05为差异有统计学意义。
2 结果
2.1 两组基线资料比较 A组男8例,女5例;年龄(63.62±14.56)岁。B组男10例,女6例;年龄(61.06±11.22)岁。两组一般资料比较,差异无统计学意义(P>0.05),具有可比性。
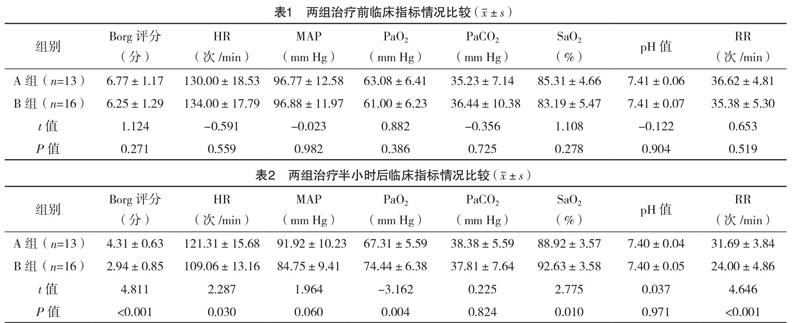
2.2 两组治疗前后的临床指标情况比较 治疗前,两组各项临床指标比较,差异均无统计学意义(P>0.05),见表1。治疗半小时后,B组HR、RR、Borg评分均低于A组,PaO2、SaO2水平均高于A组,差异均有统计学意义(P<0.05);但两组MAP、pH、PaCO2水平比较,差异均无统计学意义(P>0.05),见表2。
2.3 两组症状缓解时间、有创通气、病死及有效情况比较 B组症状缓解时间短于A组(P<0.05),两组有创通气率、病死率、有效率比较,差异均无统计学意义(P>0.05),见表3。
3 讨论
到急诊科就诊的ACPE患者,治疗上除了给予常规的强心、利尿、血管活性药物、病因治疗之外,通常还包括经鼻导管氧疗、面罩氧疗、NIPPV及气管插管机械通气等[2,7]。ACPE常因急性左心功能不全、左房及肺循环淤血、肺泡和/或肺间质水肿、肺泡表面活性物质破坏、肺顺应性下降,从而导致患者肺通气/血流比例失调,出现呼吸困难、呼吸窘迫的一组症状群,多表现为严重的低氧血症,少部分患者可合并二氧化碳潴留。因此纠正低氧血症是治疗肺水肿最基本的重要环节。HFNC作为一种新型的NIPPV模式,研究发现,其可显著改善低氧性呼吸衰竭患者的氧合指标和RR[8-11]。但对于ACPE是否有效,还有待进一步的研究。
本研究结果显示,治疗半小时后,B组HR、RR、Borg评分均低于A组,PaO2、SaO2水平均高于A组,差异均有统计学意义(P<0.05),且B组症状缓解时间短于A组(P<0.05)。这表明HFNC能快速改善ACPE患者的氧合情况,缓解呼吸困难症状。ACPE患者的毛细血管压升高、肺间质及肺泡内急性肺水肿、肺泡通气/血流比值失调、肺内分流增加、肺弥散功能和换气功能障碍、动脉血氧分压下降、缺氧,常会引起Ⅰ型呼吸衰竭,Ⅰ型呼吸衰竭不仅使组织器官缺氧,而且可引起心功能进一步恶化,心功能不全又可加重呼吸衰竭,互为因果,恶性循环[12-13]。而HFNC不仅能提供高流量湿化、加温的氧气,舒适度高,而且能产生一定的气道正压。而气道正压通气可使患者胸膜腔内压增高,减少左心室跨压,减少回心血量,从而减少心脏的前后负荷。同时可扩张陷闭肺泡,增加呼气末肺容量,改善肺的顺应,使肺泡内的水分向肺间质移动,促进肺泡液和间质液回流入血管腔,减少血管外肺积水(EVLW),使功能残气量增大,防止肺泡或小气道萎陷,改善通气/血流比例失调情况,增加氧合[14]。国外有研究报道,HFNC流量在40 L/min时,成年男性闭口时气道内呼气末正压可达PEEP 4.1 cm H2O,张口时为2.0 cm H2O;女性闭口时为7.2 cm H2O,张口时为2.3 cm H2O,且随着流量上升而上升[15]。
HFNC通过无须密闭的鼻导管直接将一定浓度的高流量空氧混合气体经过加温加湿输送给患者的一种新型无创通气氧疗方式。近年来,在成人患者,尤其在ICU应用广泛,主要针对急性呼吸衰竭、慢性阻塞性肺疾病(COPD)、围手术期患者,HFNC在成人低氧血症患者中逐渐成为NIPPV之外的选择[16-18]。由此可见,HFNC不仅能改善呼吸衰竭患者的氧合和通气,对急性心功能不全的患者也具有一定的臨床疗效。但本研究尚存在诸多局限性和不足。首先,本研究样本数量较少,只有29例,对病死率、有效率等的统计分析等有一定影响;其次,对患者的病因及基础疾病未进行分层分析比较;再者,本研究并未进行动态血流动力学和呼吸功能的监测,还需进一步的完善和改进。
綜上所述,HFNC能快速改善ACPE患者的临床指标,缓解呼吸困难症状,故HFNC可能是治疗ACPE的有效辅助手段。
参考文献
[1] Schmickl C N,Pannu S,Al-Qadi M O,et al.Decision support tool for differential diagnosis of Acute Respiratory Distress Syndrome(ARDS)vs Cardiogenic Pulmonary Edema(CPE):a prospective validation and meta-analysis[J].Crit Care,2014,18(6):659-667.
[2] Pagano A,Numis F G,Rosato V,et al.Pressure support ventilation vs Continuous positive airway pressure for treating of acute cardiogenic pulmonary edema:A pilot study[J].Respir Physiol Neurobiol,2018,255(4):7-10.
[3] Lee J H,Rehder K J,Williford L,et al.Use of high flow nasal cannula in critically ill infants,children,and adults:a critical review of the literature[J].Intensive Care Med,2013,39(2):247-257.
[4] Nishimura M.High-flow nasal cannula oxygen therapy in adults:Physiological benefits,indication,clinical benefits,and adverse effects[J].Respir Care,2016,61(4):529-541.
[5] Sitthikarnkha P,Samransamruajkit R,Prapphal N,et al.High-Flow Nasal Cannula versus Conventional Oxygen Therapy in Children with Respiratory Distress[J].Indian J Crit Care Med,2018,22(5):321-325.
[6] Chen Y Y,Chen Y,Liang S M,et al.Prognostic Impact of Fasting Plasma Glucose on Mortality and Re-Hospitalization in Patients with Acute Heart Failure[J].Chin Med J(Engl),2018,131(17):2032-2040.
[7] Plate J D J,Leenen L P H,Platenkamp M,et al.Introducing high-flow nasal cannula oxygen therapy at the intermediate care unit:expanding the range of supportive pulmonary care[J].Trauma Surg Acute Care Open,2018,3(1):1-6.
[8] Schwabbauer N,Berg B,Blumenstock G,et al.Nasal high-flow oxygen therapy in patients with hypoxic respiratory failure:effect on functional and subjective respiratory parameters compared to conventional oxygen therapy and non-invasive ventilation(NIV)[J].BMC Anesthesiol,2014,14(6):66-74.
[9] Long B,April M D.Is High-Flow Nasal Cannula More Effective Than Conventional Oxygen Therapy for Preventing Escalation of Respiratory Support in Patients With Acute Respiratory Failure[J].Ann Emerg Med,2018,72(6):716-718.
[10] Kim E S,Lee H,Kim S J,et al.Effectiveness of high-flow nasal cannula oxygen therapy for acute respiratory failure with hypercapnia[J].J Thorac Dis,2018,10(2):882-888.
[11] Azoulay E,Lemiale V,Mokart D,et al.High-flow nasal oxygen vs.standard oxygen therapy in immunocompromised patients with acute respiratory failure:study protocol for a randomized controlled trial[J].Trials,2018,19(1):157-164.
[12] Marenzi G,Cosentino N,Milazzo V.Prognostic Value of the Acute-to-Chronic Glycemic Ratio at Admission in Acute Myocardial Infarction:A Prospective Study[J].Diabetes Care,2018,41(4):847-853.
[13] Masip J,Peacock W F,Price S,et al.Indications and practical approach to non-invasive ventilation in acute heart failure[J].Eur Heart J,2018,39(1):17-25.
[14] Maraffi T,Brambilla A M,Cosentini R.Non-invasive ventilation in acute cardiogenic pulmonary edema:how to do it[J].Intern Emerg Med,2018,13(1):107-111.
[15] Ischaki E,Pantazopoulos I,Zakynthinos S.Nasal high flow therapy:a novel treatment rather than a more expensive oxygen device[J].Eur Respir Rev,2017,26(145):28-36.
[16] Sitthikarnkha P,Samransamruajkit R,Prapphal N,et al.High-Flow Nasal Cannula versus Conventional Oxygen Therapy in Children with Respiratory Distress[J].Indian J Crit Care Med,2018,22(5):321-325.
[17] Murki S,Singh J,Khant C,et al.High-Flow Nasal cannula versus Nasal Continuous Positive Airway Pressure for Primary Respiratory Support in Preterm Infants with Respiratory Distress:A Randomized Controlled Trial[J].Neonatology,2018,113(3):235-241.
[18] Miguel-Montanes R,Hajage D,Messika J,et al.Use of high flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia[J].Crit Care Med,2015,43(3):574-583.
(收稿日期:2018-07-27) (本文編辑:董悦)

