不同麻醉药物行全身麻醉复合硬膜外阻滞对肝脏切除术后肝肾功能的影响
蔡晓飞 牛少宁 丁 乔 程 灏
(首都医科大学附属北京地坛医院麻醉科,北京 100015)
· 麻醉学与神经科学 ·
不同麻醉药物行全身麻醉复合硬膜外阻滞对肝脏切除术后肝肾功能的影响
蔡晓飞 牛少宁 丁 乔 程 灏*
(首都医科大学附属北京地坛医院麻醉科,北京 100015)
目的 探讨不同麻醉药物行全身麻醉复合硬膜外阻滞对肝脏切除术后肝肾功能的影响。方法 选取首都医科大学附属北京地坛医院2014年10月至2015年10月全身麻醉复合硬膜外阻滞下肝脏切除术病人123例。采用数字表法随机抽样将研究对象分为3组(每组41例),A组病人采用七氟醚吸入全身麻醉,B组病人采用异氟醚吸入全身麻醉,C组病人采用丙泊酚静脉全身麻醉,比较3组病人不同时间点肝肾功能指标。结果 术后3组病人丙氨酸氨基转移酶(alanine aminotransferase,ALT)、门冬氨酸氨基转移酶(aspartate transaminase,AST)、碱性磷酸酶(alkaline phosphatase,ALP)、总胆红素(total bilirubin,TBiL)、γ-谷氨酰转肽酶(γ-glutamyltranspeptidase,γ-GT)、尿素氮(urea nitrogen,BUN)、血肌酐(serum creatinine,SCr)、α1-微球蛋白(α1-microglobulin,α1-MG)、白蛋白(albumin,ALB)、乳酸脱氢酶(lactic dehydrogenase,LDH)均表现为升高后降低(P<0.05)。B组病人术后1、3 d时ALT、AST、ALP、TBiL、γ-GT、BUN、SCr、α1-MG、ALB、LDH高于A组,差异有统计学意义(P<0.05)。C组病人术后1 d、3 d时ALT、AST、ALP、TBiL、γ-GT、BUN、SCr、α1-MG、ALB、LDH高于A组和B组,差异有统计学意义(P<0.05)。结论 肝脏切除术中,七氟醚、异氟醚、丙泊酚均可用于全身麻醉复合硬膜外阻滞。七氟醚对病人术后肝肾功能的影响更小,安全性更高。
七氟醚;异氟醚;丙泊酚;肝脏切除术;肝肾功能
近年来,随着饮食结构改变和人口老龄化发展,各种肝病频发[1-2],治疗方法各异,其中手术治疗较为常见,肝脏切除术是临床治疗肝脏疾病的常见外科术式[3-4]。目前,临床常用的全身麻醉药物为七氟醚、异氟醚、丙泊酚等,均可用于麻醉维持[5-7]。本课题的目的是探讨不同麻醉药物行全身麻醉复合硬膜外阻滞对肝脏切除术后肝肾功能的影响。
1 资料与方法
1.1 一般资料
选择首都医科大学附属北京地坛医院2014年10月至2015年10月肝脏切除术病人123例,入选标准:病人均行全身麻醉复合硬膜外阻滞,并由同一组医生实施相同术式,病人签署知情同意书。本项目经医院伦理委员会通过。排除标准:患有器质性疾病(除肝脏疾病外)、免疫系统疾病、血液系统疾病、精神性疾病、麻醉药物过敏的病人。采用数字表法随机抽样将病人分为3组(每组41例),A组男性28例,女性13例,年龄为48~71(61.2±4.9)岁;B组男性27例,女性14例,年龄为47~72(61.3±5.2)岁;C组男性26例,女性15例,年龄为46~73(61.0±6.4)岁,3组病人性别、年龄比较,差异无统计学意义(P>0.05),3组之间均衡可比。
1.2 方法
病人入室后,建立静脉输液通路,实施心电监护,监测血压、心率、呼吸频率、血氧饱和度等指标。依次给予病人咪达唑仑0.05 mg/kg、舒芬太尼5 μg/kg、丙泊酚1.5 mg/kg、维库溴铵0.15 mg/kg。之后行气管插管,顺利完成后给予病人机械通气以辅助呼吸,调节呼吸参数如下:潮气量为8~10 mL/kg,呼吸频率为10~12次/min,采用麻醉气体监护仪监测呼出气体浓度,维持PET CO2在35~45 mmHg(1 mmHg=0.133 kPa)之间。麻醉维持时,A组病人采用七氟醚治疗,B组病人采用异氟醚治疗,C组病人采用丙泊酚治疗。
于不同时间点行肝功能指标[丙氨酸氨基转移酶(alanine aminotransferase,ALT)、门冬氨酸氨基转移酶(aspartate transaminase,AST)、碱性磷酸酶(alkaline phosphatase,ALP)、总胆红素(total bilirubin,TBiL)、γ-谷氨酰转肽酶(γ-glutamyltranspeptidase,γ-GT)]、肾功能指标[尿素氮(urea nitrogen,BUN)、血肌酐(serum creatinine,SCr)、α1-微球蛋白(α1-microglobulin,α1-MG)、白蛋白(albumin,ALB)、乳酸脱氢酶(lactic dehydrogenase,LDH)]检测。
1.3 统计学方法

2 结果
2.1 3组病人不同时间点肝功能指标比较
术后,3组病人ALT、AST、ALP、TBiL、γ-GT均表现为升高后降低(P<0.05)。B组病人术后1 d、3 d时ALT、AST、ALP、TBiL、γ-GT高于A组,差异有统计学意义(P<0.05)。C组病人术后1 d、3 d时ALT、AST、ALP、TBiL、γ-GT高于A组和B组,差异有统计学意义(P<0.05)。详见表1。
2.2 3组病人不同时间点肾功能指标比较
术后,3组病人BUN、SCr、α1-MG、ALB、LDH均表现为升高后降低(P<0.05)。B组病人术后1 d、3 d时BUN、SCr、α1-MG、ALB、LDHT高于A组,差异有统计学意义(P<0.05)。C组病人术后1 d、3 d时BUN、SCr、α1-MG、ALB、LDH高于A组和B组,差异有统计学意义(P<0.05)。详见表2。
3 讨论
肝脏切除术是临床常用术式,主要应用于肝癌,其次是良性肿瘤,两者约占肝切除病例的80%[8-9]。其他适应证包括肝内胆管结石、肝外伤、肝脓肿和不适合引流的包囊虫囊肿等,可行部分肝切除术。根据病变的范围大小和位置行楔行切除、肝局部切除、左半肝或右半肝切除。肝切除目前是治疗肝癌的首选方法,特别是早期肝癌,手术切除术的远期疗效较其他任何方法都好[10-11]。
手术操作需要给予病人麻醉,目前常用方法为全身麻醉复合硬膜外阻滞[12-13]。该方法可以显著减少麻醉药物用量,对手术操作中产生的应激反应也会有明显的抑制效果,能够有效维持机体心肌供氧量,将有助于促进病人的术后恢复。全身麻醉复合硬膜外阻滞会对病人的血流动力学指标产生不同程度的影响,其中肝功能指标与肾功能指标的改变比较明显。分析麻醉用药如下:七氟醚首先由Ross Terrell发现,于1968年由Regan合成,1986年完成三期临床试验,1990年首先由日本的药监部门批准临床使用[14]。近年来,被许多著名麻醉学专家誉为吸入麻醉的里程碑式药物,并认为在儿童全麻诱导及其维持中有显著优点,也有许多研究[15-16]报道了将其广泛用于儿童全麻的成功经验。七氟醚诱导时间比较短,麻醉期间的镇痛、肌松效应较好,呼吸抑制作用较小,对心血管系统的影响较小,对脑血流量、颅内压的影响也较小,安全性较高。
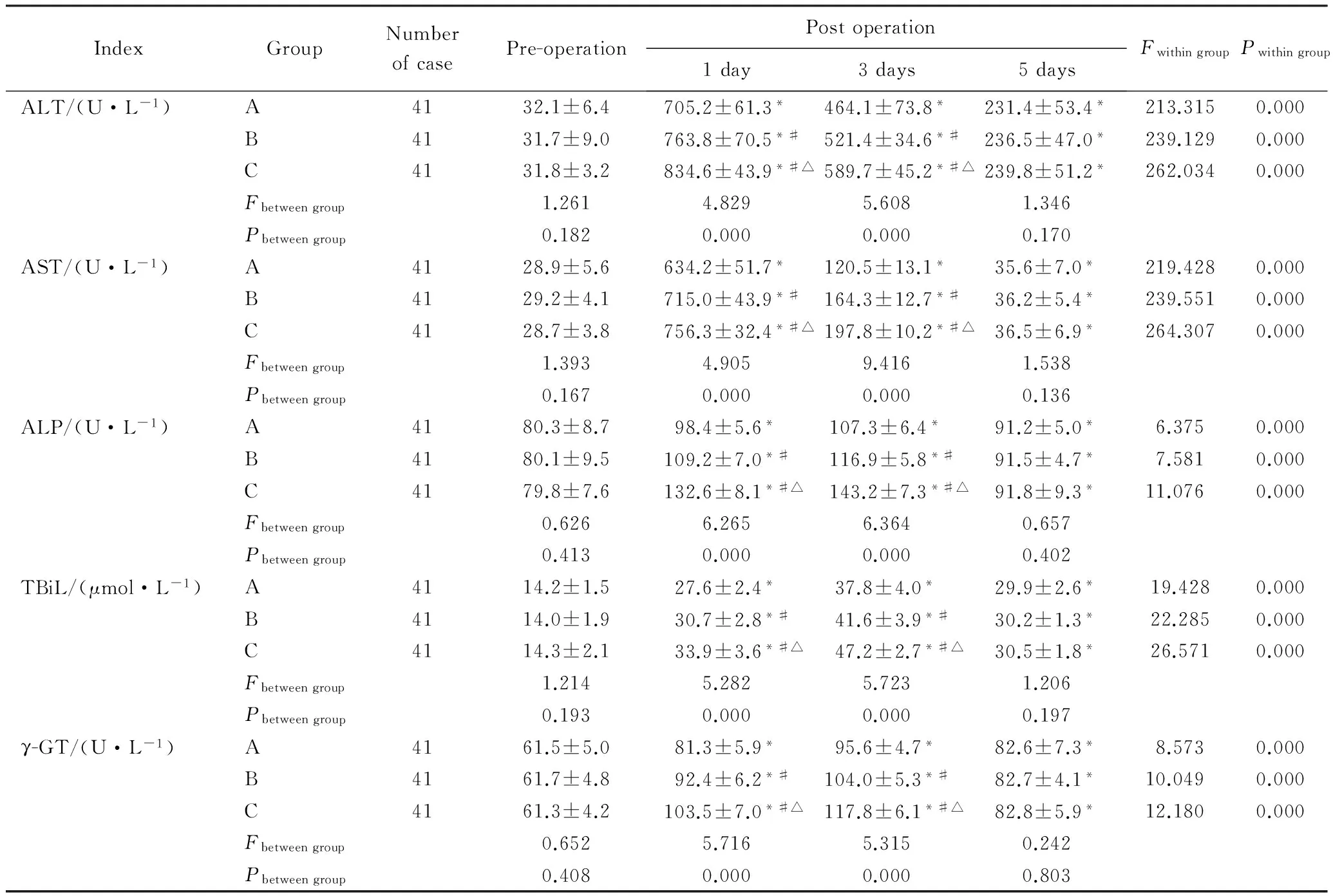
表1 3组病人不同时间点肝功能指标比较Tab. 1 Comparison of liver function tests at different time points among the three groups
*P<0.05vspre-operation,#P<0.05vsgroup A,△P<0.05vsgroup B;ALT:alanine aminotransferase;AST:aspartate transaminase;ALP:alkaline phosphatase; TBiL: total bilirubin;γ-GT: γ-glutamyltranspeptidase.
异氟醚是一种带乙醚样气味的无色澄明液体,是恩氟烷的异构体,吸入后药物浓度在血中迅速达到平衡,肺泡内浓度很快上升并接近吸入气浓度,故诱导迅速,苏醒亦快[17-18]。异氟醚对中枢神经系统可产生进行性下行性抑制,脑耗氧量减少,脑血流量增多及颅内压上升,但过度通气即可纠正。异氟醚能抑制神经肌肉接头,肌松良好。对循环系统和呼吸系统的抑制作用小,对呼吸道黏膜几无刺激性,并可扩张收缩的支气管。
丙泊酚是目前临床上普遍用于麻醉诱导、麻醉维持、重症监护病房(intensive care unit, ICU)危重病人镇静的一种新型快速、短效静脉麻醉药,具有麻醉诱导起效快、苏醒迅速且功能恢复完善,术后恶心呕吐发生率低等优点[19-20]。丙泊酚为烷基酚类的短效静脉麻醉药,通过激活γ-氨基丁酸(gamma-aminobutyric acid, GABA)受体-氯离子复合物,发挥镇静催眠作用。临床剂量时,丙泊酚增加氯离子传导,大剂量时使GABA受体脱敏感,从而抑制中枢神经系统,产生镇静、催眠效应,起效快,作用时间短,苏醒迅速。丙泊酚能抑制咽喉反射,有利于插管,很少发生喉痉挛。对循环系统有抑制作用,可引起血压下降,心肌血液灌注及氧耗量下降,外周血管阻力降低,心率无明显变化,安全性很高。
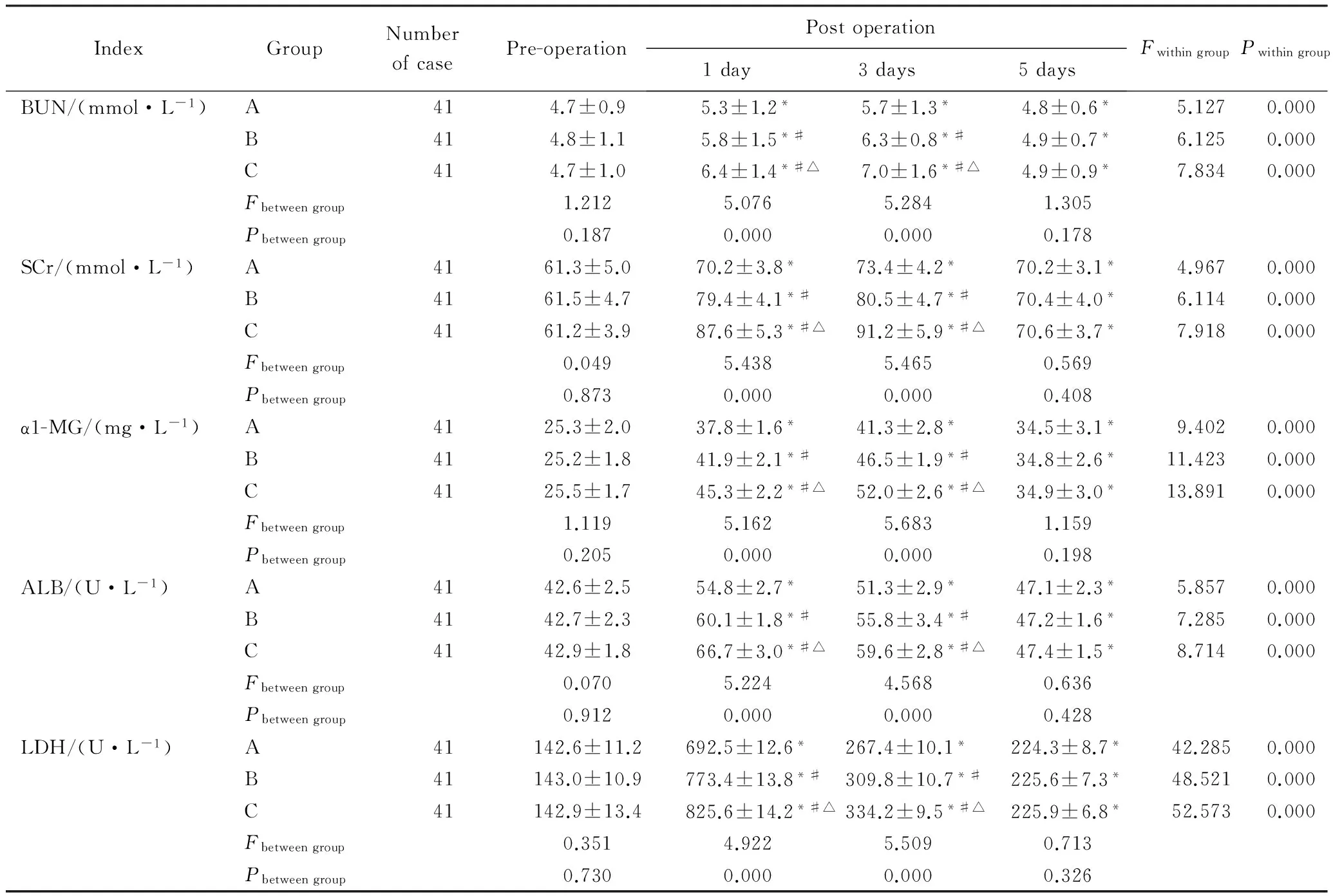
表2 3组病人不同时间点肾功能指标比较Tab.2 Comparison of kidney function tests at different time points among the three groups
*P<0.05vspre-operation;#P<0.05vsgroup A;△P<0.05vsgroup B; BUN:urea nitrogen; SCr:serum creatinine,SCr;α1-MG:α1-microglobulin; ALB:albumin;LDH: lactic dehydrogenase.
此次研究筛选的病例较为严格,在病人一般情况、术式、手术切除部位、手术时长、出血量、麻醉复苏时间等各种参考因素上都大致相同,在数据上差异无统计学意义,术前均无合并症,术后未出现手术及麻醉相关合并症,在数据上差异也无统计学意义。因文章内容所限,未做深入讨论。因此考虑3组数据的对比已基本排除了其他因素对结果的影响,麻醉药物种类的不同是造成肝肾功能指标差异的主要原因,所以认为3组比较还是有临床价值的,如果扩大样本范围可能效果更显著,对肝脏切除术的麻醉用药更加有指导意义。
本次研究结果显示,术后3组病人ALT、AST、ALP、TBiL、γ-GT均表现为升高后降低(P<0.05)。B组病人术后1 d、3 d时ALT、AST、ALP、TBiL、γ-GT高于A组(P<0.05)。C组病人术后1 d、3 d时ALT、AST、ALP、TBiL、γ-GT高于A组和B组(P<0.05)。说明肝脏切除术中,七氟醚、异氟醚、丙泊酚均可用于全身麻醉复合硬膜外阻滞。其中七氟醚对病人术后肝功能的影响更小,安全性更高。
术后,3组病人BUN、SCr、α1-MG、ALB、LDH均表现为升高后降低(P<0.05)。B组病人术后1 d、3 d时BUN、SCr、α1-MG、ALB、LDHT高于A组(P<0.05)。C组病人术后1 d、3 d时BUN、SCr、α1-MG、ALB、LDH高于A组和B组(P<0.05)。说明七氟醚对病人术后肾功能的影响也较小,有助于改善病人的预后,效果显著,值得临床推广使用。但此次研究存在一定弊端,样本量较少,需要进一步扩大样本量再进行探讨。
[1] Young J, Weis N, Hofer H, et al. The effectiveness of daclatasvir based therapy in european patients with chronic hepatitis C and advancedliver disease[J]. BMC Infect Dis, 2017, 17(1):45.
[2] Tu J, Jia Z, Ying X, et al. The incidence and outcome of major complication following conventional TAE/TACE for hepatocellular carcinoma[J]. Medicine (Baltimore), 2016, 95(49):e5606.
[3] Zhong J H, Peng N F, Gu J H, et al. Is laparoscopic hepatectomy superior to open hepatectomy for hepatocellular carcinoma?[J]. World J Hepatol, 2017, 9(4):167-170.
[4] Kim C W, Lee J L, Yoon Y S, et al. Resection after preoperative chemotherapy versus synchronous liver resection of colorectal cancer livermetastases: a propensity score matching analysis[J]. Medicine (Baltimore), 2017, 96(7):e6174.
[5] Munmany M, Gracia M, Nonell R, et al. The use of inhaled sevoflurane during operative hysteroscopy is associated with increased glycine absorption compared to intravenous propofol for maintenance of anesthesia [J]. J Clin Anesth, 2016,31(1): 202-207.
[6] Raisis A L, Smart L, Drynan E, et al. Cardiovascular function during maintenance of anaesthesia with isoflurane or alfaxalone infusionin greyhounds experiencing blood loss [J]. Vet Anaesth Analg, 2015, 42(2):133-141.
[7] Caines D, Sinclair M, Valverde A, et al. Comparison of isoflurane and propofol for maintenance of anesthesia in dogs with intracranial disease undergoing magnetic resonance imaging [J]. Vet Anaesth Analg, 2014, 41(5):468-479.
[8] Ohmura Y, Takeda Y, Katsura Y, et al. Laparoscopic Liver Resection for Elderly Patients with HCC[J]. Gan To Kagaku Ryoho, 2016, 43(12):1518-1520.
[9] Kim W J, Kim K H, Shin M H, et al. Totally laparoscopic anatomical liver resection for centrally located tumors: A single center experience[J]. Medicine (Baltimore), 2017, 96(4):e5560.
[10]Haga S, Yimin, Ozaki M. Relevance of FXR-p62/SQSTM1 pathway for survival and protection of mouse hepatocytes and liver, especially with steatosis[J]. BMC Gastroenterol, 2017, 17(1):9.
[11]Dedinská I, Laca L, Miklušica J, et al. Complications of liver resection in geriatric patients[J]. Ann Hepatol, 2017, 16(1):149-156.
[12]Xu Y, Sun Y, Chen H, et al. Effects of two different anesthetic methods on cellular immunity of patients after liver cancer resection[J]. J Biol Regul Homeost Agents, 2016, 30(4):1099-1106.
[13]Siniscalchi A, Gamberini L, Bardi T, et al. Role of epidural anesthesia in a fast track liver resection protocol for cirrhotic patients-results after three years of practice[J]. World J Hepatol, 2016, 8(26):1097-1104.
[14]Terrell R C. The invention and development of enflurane, isoflurane, sevoflurane, and desflurane[J]. Anesthesiology, 2008, 108(3):531-533.
[15]Kang D X, Rao Y Q, Ji B, et al. Effects of sevoflurane and desflurane on pharmacodynamics of rocuronium in children[J]. Zhonghua Yi Xue Za Zhi, 2017, 97(6):429-433.
[16]Cornelissen L, Bergin A M, Lobo K, et al. Electroencephalographic discontinuity during sevoflurane anesthesia in infants and children[J]. Paediatr Anaesth, 2017, 27(3):251-262.
[17]Menting T P, Ergun M, Bruintjes M H, et al. Repeated remote ischemic preconditioning and isoflurane anesthesia in an experimental model of renal ischemia-reperfusion injury[J]. BMC Anesthesiol, 2017, 17(1):14.
[18]Hambrecht-Wiedbusch V S, Li D, Mashour G A. Paradoxical emergence: administration of subanesthetic ketamine during isoflurane anesthesia induces burst suppression but accelerates recovery[J]. Anesthesiology, 2017, 126(3):482-494.
[19]Mir A H, Shah N F, Din M U, et al. Effectiveness of sodium thiopentone, propofol, and etomidate as an ideal intravenous anesthetic agent for modified electroconvulsive therapy[J]. Saudi J Anaesth, 2017, 11(1):26-31.
[20]Pan J R, Cai J, Zhou S L, et al. Pharmacodynamic analysis of target-controlled infusion of propofol in patients with hepatic insufficiency[J]. Biomed Rep, 2016, 5(6):693-698.
编辑 孙超渊
Influence of general anesthesia combined with epidural block on liver and kidney function after liver resection
Cai Xiaofei, Niu Shaoning, Ding Qiao, Cheng Hao*
(DepartmentofAnesthesiology,BeijingDitanHospital,CapitalMedicalUniversity,Beijing100015,China)
Objective To explore the influence of different anesthetic drugs for general anesthesia combined with epidural block on liver and kidney function after liver resection. Methods Totally 123 patients with liver resection were selected from Beijing Ditan Hospital who underwent general anesthesia combined with epidural block from October 2014 to October 2015. Patients were divided into three groups by simple random sampling. Forty-one patients were treated with sevoflurane as group A. Another 41 patients were treated with isoflurane as group B. Additional 41 patients were treated with propofol as group C. The result of liver and kidney function tests at different time points were compared among the three groups. Results After operation,alanine aminotransferase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), total bilirubin (TBiL), γ-glutamyltranspeptidase (γ-GT), urea nitrogen (BUN), serum creatinine (SCr), α1-microglobulin (α1-MG), albumin (ALB), lactic dehydrogenase (LDH) increased firstly and then decreased in each of the three groups(P<0.05). ALT, AST, ALP, TBiL, γ-GT, BUN, SCr, α1-MG, ALB, LDH at postoperative day 1, day 3 in group B were higher than those of group A(P<0.05). ALT, AST, ALP, TBiL, γ-GT, BUN, SCr, α1-MG, ALB, LDH at postoperative day 1, day 3 in group C were higher than those of group A and B(P<0.05). Conclusion In liver resection, sevoflurane, or isoflurane, propofol can be used for general anesthesia combined with epidural block. Sevoflurane showed less effect on liver and kidney function, and had more safety profile.
sevoflurane; isoflurane; propofol; liver resection; liver and kidney function
首都医科大学附属北京地坛医院院内“启航计划”(DTQH201405)。 This study was supported by “Sailing Plan” of Beijing Ditan Hospital of Capital Medical University(DTQH201405).
时间:2017-06-09 17∶26 网络出版地址:http://kns.cnki.net/kcms/detail/11.3662.r.20170609.1726.014.html
10.3969/j.issn.1006-7795.2017.03.005]
R614
2017-03-20)
*Corresponding author, E-mail:chenghaocn@yahoo.com