Efficacy of Willis covered stent of intracranial pseudoaneurysms in the internal carotid artery: A systematic review and meta-analysis
Li Lin ,Shao-Wei Xiang ,Yan-Ling Sun ,Yuan Chen ,Zhe Wu ,Zhi-Feng Ning ,Ding-Wen Shen,Xue-Qin Sima✉,Qi-Qiang Wen,Gui-Lai Wei,Qing-Yong He
1Department of Biochemistry,Basic School School,Hubei University of Science and Technology,Xianning City,Hubei Province 437100,China
2The Third Surgery Department,Enshi State Central Hospital,Enshi State,Hubei Province 445000,China
3Department of Histology and Embryology,Basic School School,Hubei University of Science and Technology,Xianning City,Hubei Province 437100,China
4Department of Cardiothoracic Surgery,Xianning Central Hospital,Hubei University of Science and Technology,Xianning City,Hubei provinceProvince 437100,China
5Department of Human Anatomy,Basic School School,Hubei University of Science and Technology,Xianning City,Hubei Province 437100,China
6Department of Parasite,Basic School School,Hubei University of Science and Technology,Xianning City,Hubei Province 437100,China
7Hubei University of Science and Technology,Xianning City,Hubei Province 437100,China
8School of Physical Education,Hubei University of Science and Technology,Xianning City,Hubei Province 437100,China
ABSTRACT Objective: To evaluate the efficacy of a novel coated stent in the treatment of intracranial pseudoaneurysm.Methods: MEDLINE,EMBASE,and PubMed databases were searched for literature published between 1990 and April 2022 according to PRISMA guidelines.All studies with ≥10 patients reporting successful implantation of Willis covered stent,therapeutic effect,complications,and postoperative follow-up were included.The combined incidence and corresponding 95% confidence intervals were assessed using a generalized linear mixed method and random effects model.Results: Five studies (116 patients with pseudoaneurysms) were included.The experimental groups in the selected studies showed a combined technical success rate of 81.03% (OR=18.31,95%CI=9.39-35.69,I2=79%,P<0.001).Clinical follow-up showed that the complete cure rate was as high as 94.4% after the follow-up(OR=106.81,95% CI=39.08-291.88,I2=0%,P=0.71).Conclusions: Willis covered stent is feasible,safe,and effective in the treatment of intracranial pseudoaneurysm.
KEYWORDS: Intracranial pseudoaneurysms;Willis covered stent;Systematic review;Meta-analysis;Internal carotid artery;Endoleak;Neurosurgery
1.Introduction
Intracranial pseudoaneurysms (PSAs) of the internal carotid artery are a rare disease in neurosurgery[1].Pseudoaneurysm of the carotid artery refers to the formation of hematoma caused by artery wall damage and blood extravasation due to various reasons.The hematoma disappeared over time.Under the impact of the continuous pulsating pressure of the artery,the hematoma communicates with the arterial cavity through the artery tear and forms a pseudoaneurysm.Traumatic PSAs in the intracranial segment of the internal carotid artery are the most common type,with an incidence of about 1% of intracranial aneurysms.At present,several factors can cause PSAs,such as trauma,infection,iatrogenic cause,or malignancy,but at present,blunt trauma and severe trauma are the most common factors causing PSA[1].
PSAs are characterized by the presence of organized hematoma and fibrosis outside the true lumen,rather than the normal vascular component,and are prone to rupture and bleeding,and other serious complications[2].PSA is formed when the artery wall completely ruptures,resulting in an extravascular hematoma connected to the ruptured artery.Thus,PSA is difficult to manage surgically due to its fragility,fusiform shape,and lack of a true neck.PSAs usually occur near pseudocysts.Pseudocysts can be transformed into PSAs by direct mass action on peripheral blood vessels.With photolytic enzymes,a pseudoaneurysm eats away at and connects to a blood vessel,forming a large pseudoaneurysm.
In recent years,microsurgical treatment has been transformed into endovascular treatment,which can effectively protect the parent artery and reduce morbidity and mortality[3].Microsurgical techniques have recently been shown to have advantages over traditional surgical procedures.Coil embolization or bare stenting or double bare stenting with or without coil embolization demonstrated immediate and short-term success in the treatment of internal carotid artery (ICA)-preserved traumatic PSAs.The use of 4-6 coils and bare stents does not always rule out pseudo malformations in the lumen of the mother vessel.It is less invasive,and its advantages are especially evident when surgery is contraindicated for various reasons.However,vascular surgery has a higher risk of intraoperative fatal bleeding and/or large vessel occlusion[4].Willis covered stent(WCS) is a balloon dilating stent specially made for intracranial vessels[5],which can prevent blood from flowing into the aneurysm cavity and retain the parent artery,thus restoring the normal vascular morphology,and is a promising device for intracranial aneurysm treatment.When real-time angiography detected residual internal leakage,balloon reflation was performed proximal and distal to the stent at 8 atmospheric pressure to ensure maximum stent expansion,thereby improving stent stability and preventing internal leakage.
For a long time,WCS has been reported as an effective method for the treatment of internal carotid aneurysms,with good safety and short-term efficacy,but its application in PSAs has only been discovered in recent years.Therefore,we performed a meta-analysis to evaluate the application effect of WCSs in PSAs.
2.Subjective and methods
2.1.Search strategy
A comprehensive search was conducted using MEDLINE,PubMed,and EMBASE for research published in the period from 1990 to 2022.We used key search terms to generate search expressions,{[“aneurysm,false” (MeSH Terms) OR [“aneurysm” (All Fields)AND “false” (All Fields)]OR “false aneurysm” (All Fields) OR[“false” (All Fields) AND “aneurysms” (All Fields)]OR “false aneurysms” (All Fields) OR [“aneurysm,false” (MeSH Terms)]OR [“aneurysm” (All Fields) AND “false” (All Fields)]OR “false aneurysm” (All Fields) OR “pseudoaneurysm” (All Fields)]} AND[willis (All Fields) AND covered (All Fields) AND [“stents” (MeSH Terms) OR “stents” (All Fields) OR “stent” (All Fields)],which helped us to screen out 202 articles in total.All literature retrieved had no language limitation.This meta-analysis was based on the PRISMA statements.
2.2.Inclusion and exclusion criteria
Inclusion criteria were as follows: 1) study sample >10 patients,2) all patients were treated with WCSs only,and 3) PSAs formation was confirmed.The exclusions were as follows based on the results of angiography: 1) complete exclusion,no residual cavity,and no internal fistula;2) incomplete exclusion,residual aneurysm cavity,and internal fistula.
2.3.Data extraction
Two radiologists independently reviewed and extracted complete data from all studies,including demographic details,whether WCSs were used,the size of PSAs,technical and clinical success rates,the incidence of postoperative internal leakage,rebreeding rates,complications,and mortality.If there is any inconsistency,it should be agreed upon after discussion with a third reviewer.
2.4.Quality assessment
The quality assessment tool of the NIH case series was used to assess the quality of the selected studies[6].Two radiologists independently reviewed the studies using the NIH Research Evaluation Tool.
2.5.Outcomes
The main outcome was complete cure rate.
2.6.Statistical analysis
RevMan5.2 software was used.We pooled data using a randomeffects meta-analysis of weighted average differences and aP=0.05 as a significance setting.Dichotomous variables were represented by odds ratio,representing 95% confidence intervals (CI).I2statistics were used to evaluate the heterogeneity of individual study results.The random effect model was used whenI2>50%,while the fixed effect model was used whenI2<50%.Funnel plots are used to screen for potential publication bias.
3.Results
3.1.Cumulative study data
A total of 202 studies were identified through the search strategy.After qualifying screening,5 studies met the final analysis of inclusion criteria[5,7-10](Figure 1).These 5 studies had 116 patients.All included studies were case-control study design (Table 1).
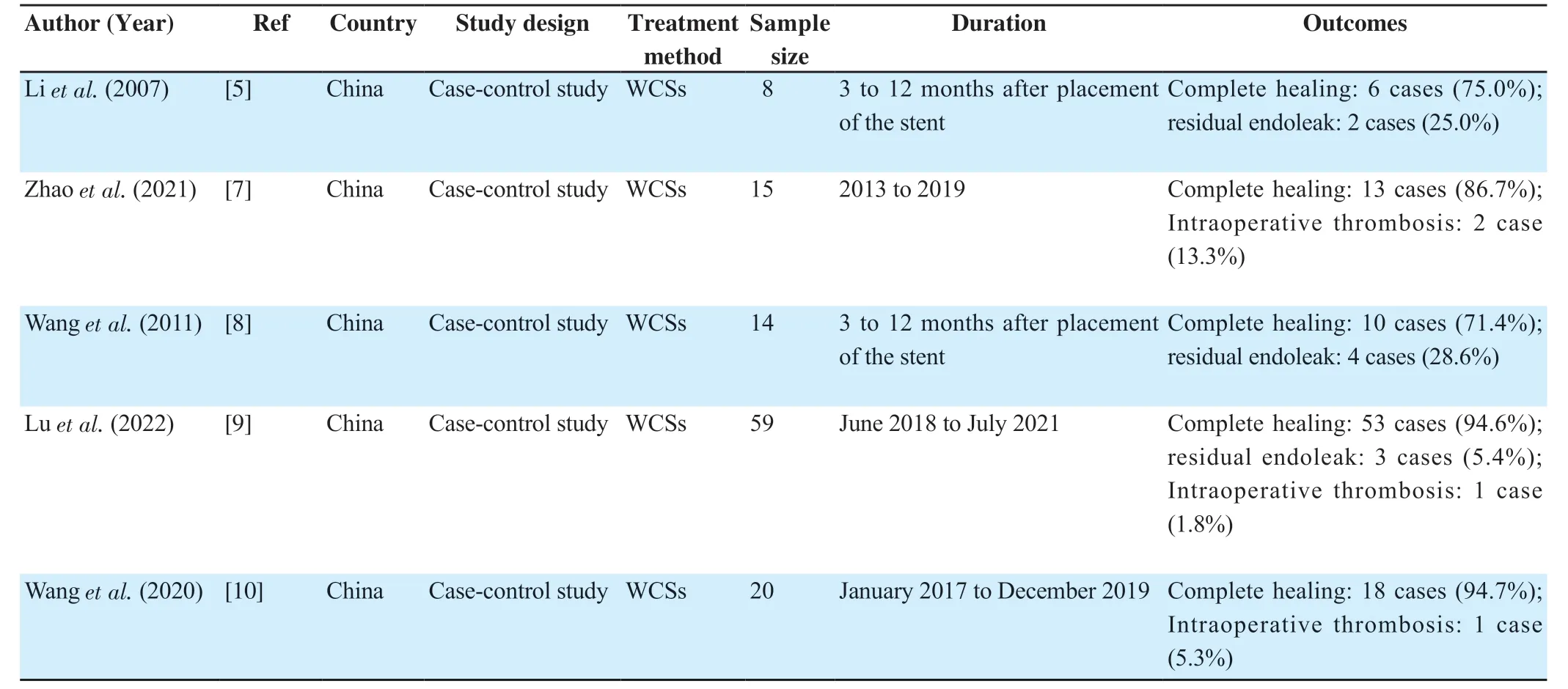
Table 1.Descriptive summary of the studies included in the meta-analysis for the association between the WCSs and PASs.

Figure 1.The study flowchart.
3.2.Combined technical success rate of WCSs in PSAs
The experimental groups in the selected studies showed a combined technical success rate of 81.03% (95%CI=9.39-35.69,I2=79%,P<0.001) (Figure 2).The random effect model was used asI2>50%.

Figure 2.Forest plot of surgical success rate after Willis covered stent implantation for pseudoaneurysms treatment.
3.3.Follow-up of patients with PASs after using WCSs
Although the majority of patients did not recover after the first operation,the majority of patients recovered spontaneously in the follow-up,with few bleeding and other complications.The data showed that the complete cure rate was significantly increased after using WCSs with the follow-up (I2=0%,P=0.71,OR=106.81,P<0.001) (Figure 3).This indicates that the implantation of WCSs in the treatment of pseudoaneurysms has a significant effect.
3.4.Publication bias
In addition,we also use a funnel plot to evaluate publication bias,which showed that publication bias existed (Figure 4).

Figure 4.Funnel plot,A: surgical success rate;B: cure rate.
4.Discussion
PSAs are called PSAs because they don’t have trivertebra walls,media,and intima,instead,they have fibrin walls,which ultimately explains why they have coil squeezing[11].The development and diagnosis of PASs lesions are often delayed[12-14].
Due to the lack of a normal artery wall,traditional interventional therapy is not effective in repairing the rupture,even at the expense of blocking the parent artery,and is not the best treatment.WCS is an ideal treatment with the advantages of immediate reconstruction of the normal vascular wall,retention of patency of the parent artery,and restoration of normal blood perfusion.WCS was designed by Liet al.[15],based on their rich experience in the treatment of cerebral aneurysms in China.WCS is the only stent system designed specifically for intracranial vessels.It is designed to seal PSAs,keep ICA open,and eliminate pathological vascular damage.To date,it has been used for the treatment of a large variety of ICA diseases[16],including traumatic pseudoaneurysm,carotid cavernous sinus fistula after balloon treatment,coiled recurrent aneurysm,and large intracranial aneurysm[17].With the increasing popularity of special intracranial stents,reconstruction methods are becoming more and more important in the treatment of PSAs[18].In this metaanalysis,we searched literature on the treatment of intracranial pseudoaneurysm with WCSs,and 116 patients with intracranial pseudoaneurysm were included.Our results indicate that the device is safe and effective in the treatment of intracranial PSAs.
However,aneurysmal leakage remains a significant problem after WCS placement because of continuous blood flow in the aneurysmal sac.The aneurysm sac is filled with coils,balloons,or fluid to keep the parent artery open,but due to the lack of a true blood vessel wall,pseudoaneurysm rupture is prone to occur during surgery[19,20].Persistent internal leakage is the main factor leading to continuous expansion or rupture of aneurysms,especially in the case of acute aneurysm rupture.The mismatch between the stent and lesion is the main cause of intraluminal leakage.Due to stent size mismatch with the mother vessel,sectional shape mismatch,possible PTFE film rupture,potential stent shortening,an uneven lumen of lesion vessels,incomplete cervical coverage of aneurysm,transient vasospasm,stent displacement,and stent rupture,WCS deployment may lead to internal leakage.
In the case of persistent internal leakage after 2-3 attempts to reinflate the balloon,the following method is used.If there was internal leakage at the distal end of the stent,the operation was stopped and angiographic follow-up was performed at least 3 months later.In the case of internal leakage at the proximal end of the stent,consider using a second covering stent.The two cover brackets must overlap by at least 3 mm,and the second bracket must be at least 0.5 mm larger than the first bracket.The patient’s signs and symptoms were monitored postoperatively until discharge.In general,proximal and distal balloon reflation of the stent inhibits most direct internal leakage events.But the incidence of internal leakage is not low.Previous reports showed that the incidence of immediate internal leakage ranged from 16% to 32%[19].A study reported that 16 cases (16/56,28.6%) had internal leakage after initial balloon expansion[20].
WCS system has been improved on the existing stent model in terms of the stent structure,membrane thickness,stent delivery system,and stent diameter or length.This has resulted in significant improvements in stent flexibility,tractability,and radiographic opacity,and remote navigation is now possible.Despite many significant improvements,there are still some side effects.Post-stent stenosis,cerebral vasospasm caused by balloon stent expansion,and collateral closure of stent-covered artery segments are common side effects.Blood bypass stents cannot immediately remove the aneurysm from circulation,and complete occlusion could occur for weeks[21].In addition,patients had a higher risk of rebreeding after subsequent antiplatelet therapy.Antiplatelet therapy is an important therapeutic strategy for the application of stents.Aspirin combined with clopidogrel dual antiplatelet therapy could achieve a satisfactory long-term patency effect.However,antiplatelet therapy presents a challenge when stent overlays are placed for PSAs,as the treatment may increase the risk of bleeding.Furthermore,both the stent and the parent artery can be damaged as the stent struggles through the twisting vessels[22].Therefore,WCS navigation still requires further attention,especially in the deep curve of the intracranial vessels[23,24].Long-term follow-ups are also needed.
Our study has several limitations.All the patients were from the same center,and there could be potential regional and ethnic selection bias.Few studies reported follow-up results.Many studies lacked important data,including arterial rebreeding (embolizationvs.new occurrence),and complications were not graded according to standard guidelines.For future studies,larger samples and longer follow-up studies are needed.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This work was supported by China Natural Science Funding (No.81902937) and Hubei University of Science and Technology ENT special project (No.2020WG06),Hubei University of Science and Technology ENT special project (No.2) and Hubei province Key R&D plan (2022BCE011) and (No.2020XZ30) for SDW,Hubei University of Science and Technology the Second Affiliated Hospital Scientific project (No.2020LCZ001) and ENT special project (No.2021WG10).
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors’ contributions
LL,XSW and CY wrote and prepared the manuscript.WZ,NZF,SDW,and WGL performed the statistical analysis.HQY,WQQ,SXQ,and SYL revised the manuscript.
 Journal of Acute Disease2023年5期
Journal of Acute Disease2023年5期
- Journal of Acute Disease的其它文章
- Intention and hesitancy to receive a booster dose of COVID-19 vaccine among pregnant women using a health belief model: A cross-sectional study
- Mechanical ventilation and outcomes in COVID-19 patients admitted to intensive care unit in a low-resources setting: A retrospective study
- Diagnostic value of ABCD2 and ABCD3-Ⅰ risk scoring systems in determining one-month risk of stroke in patients with transient ischemic attack: An observational study
- Cardiovascular sequelae in post-COVID-19 patients with moderate to severe CT severity score: A follow-up study
- Pathological and immunohistochemical findings of lungs,heart,liver,and kidneys,and unexpected findings of fungi and parasites in lungs of deceased COVID-19 patients: A case series
- Penetrating soft palate injury by lollypop candy stick
