Pathological and immunohistochemical findings of lungs,heart,liver,and kidneys,and unexpected findings of fungi and parasites in lungs of deceased COVID-19 patients: A case series
Mehmet N.Yakar ,Bişar Ergün ,Aylin Erol ,Özde Gökbayrak ,Tekincan Ç.Aktaş ,Özlem Ulusan Bağcı ,Fırat Bayraktar,Eyüp S.Uçan,Begüm Ergan,Bilgin Cömert,Ayşe Caner,Safiye Aktaş,Ali N.Gökmen
1Division of Intensive Care,Department of Anaesthesiology and Reanimation,Faculty of Medicine,Dokuz Eylül University,İzmir,Turkey
2Division of Intensive Care,Department of Internal Medicine,Faculty of Medicine,Dokuz Eylül University,İzmir,Turkey
3Department of Basic Oncology,Institute of Oncology,Dokuz Eylül University,İzmir,Turkey
4Department of Basic Oncology,Institute of Health Sciences,&5Department of Parasitology,Faculty of Medicine,Ege University,İzmir,Turkey
6Division of Endocrinology and Metabolic Diseases,Department of Internal Medicine,Faculty of Medicine,Dokuz Eylül University,İzmir,Turkey
7Department of Chest Diseases,Faculty of Medicine,Dokuz Eylül University,İzmir,Turkey
ABSTRACT Objective: To define histopathologic and immunohistochemical features of the lungs,heart,liver,and kidneys in patients who died from coronavirus disease 2019 (COVID-19),and to determine the presence of SARS-CoV-2 in all tissues,as well as the presence of fungi and parasites in lung tissues.Methods: This retrospective case study was conducted in the intensive care units of Dokuz Eylül University Hospital,and patients(≥18 years) who died due to COVID-19 between October 2020 and April 2021 were included.The biopsy samples of the patient’s lung,heart,liver,and kidney tissues were studied.Results: In the study,we enrolled 12 patients (mean age: 70 years;50% male).Alveolar epithelial cell damage and diffuse alveolar damage were predominant in lung tissues.Lobular lymphocyte infiltration,centrilobular sinusoidal dilatation,and microvesicular steatosis in the liver,together with pigmented cast,non-isometric vacuolar degeneration,and capillary plugging in the kidneys,were commonly found among the patients.SARS-CoV-2 nucleocapsid protein antibodies were detected in three lung and two kidney tissues,and so did angiotensin-converting enzyme 2 receptor positivity in one lung and more than half of the kidney tissues.The RT-PCR tests were positive in three lungs and one kidney tissue.After DNA isolation from lung tissues,Pneumocystis jirovecii was detected in nine patients,Aspergillus fumigatus in two,Microsporidia in three,and Cryptosporidium in two.Conclusions: SARS-CoV-2 is a multisystemic disease.Fungi and parasites should be investigated in critically ill COVID-19 patients prescribed corticosteroids.
KEYWORDS: Biopsy;COVID-19;Histopathology;Immunohistochemistry;Opportunistic infections;SARS-CoV-2
1.Introduction
Coronavirus disease 2019 (COVID-19) was a pandemic resulting in millions of infected cases and deaths[1],despite the many treatment modalities[2-4].Possible pathophysiological mechanisms,organ injuries,and direct cellular effects of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were intensely debated in the literature.Several researchers defined the histopathologic features of the disease in biopsies sampled from various organs and autopsy series.However,multiorgan pathological evaluation is limited in the literature[5,6].Furthermore,the pathophysiological mechanisms of COVID-19-related organ injuries and histopathologic findings in various organs remain unclear[7-9].Additionally,previous studies revealed that the use of corticosteroids or cytokine blockers for the prevention of hyperimmune response and cytokine storm[3,4]might cause opportunistic infections,including fungal,parasitic,and viral agents[10].
In this clinicopathologic study,critically ill patients with a laboratory-confirmed diagnosis of COVID-19 were evaluated and the patients’ clinical characteristics and laboratory data were studied for histopathologic and immunohistochemical findings in lung,heart,liver,and kidney tissues.The presence of SARS-CoV-2 was investigated in all tissues,as well as fungi and parasites in lung biopsy samples using the real-time polymerase chain reaction test(RT-PCR) after DNA isolation.The present study aims to identify pathological and immunohistochemical findings in patients who died from COVID-19 and to determine opportunistic infection agents in the lungs.
2.Patients and methods
2.1.Study setting and design
Critically ill patients (≥ 18 years) with a laboratory-confirmed diagnosis of COVID-19 by RT-PCR test on respiratory samples and who died from COVID-19 in the intensive care units (ICU) of Dokuz Eylül University Hospital between October 2020 and April 2021 were enrolled in the study.
2.2.Ethical approval
This retrospective study (Clinical Trials.gov identifier:NCT04678687) was conditionally approved by the local ethics committee of Dokuz Eylül University (date: 26/06/2020,IRB:520-SBKAEK) after the pre-approval by the Ministry of Health of the Republic of Turkey (date: 27/05/2020).Final approval was given by the Turkish Medicines and Medical Devices Agency (date:01/09/2020,number: 66175679-514.99-E.197314).The study was conducted in the ICUs of Dokuz Eylül University Hospital.Written informed consent was obtained from the patients’ next of kin and the study was performed following the ethical standards described in the version of the 1975 Declaration of Helsinki,as revised in 2013[11].
2.3.Biopsy sampling
2.3.1.Biopsy
Biopsy procedures were performed in the isolated rooms inside the ICU under personal protective equipment within the first hour of death.In all cases,the procedure was performed by two trained intensivists using disposable automatic tru-cut biopsy instruments(14-gauge,15 cm) under ultrasound guidance for heart,liver,and kidney biopsies.Biopsy forceps (2.3 mm,230 cm) or automatic Tru-Cut biopsy instruments (14-gauge,15 cm) were used for transtracheal or transthoracic lung biopsies.The biopsy samples were immediately fixed into 10% neutral-buffered formalin on sampling time.
2.3.2.Pathological and immunohistochemical evaluation
All lung,heart,liver,and kidney biopsy samples were kept in 10% neutral-buffered formalin for 48 hours.Biopsy specimens were blocked after 24 hours of standard tissue processing in the tissue processor device (Indesit Company,Fabriano,Ancona,Italy).Paraffin-embedded specimens were sectioned at 3 μm by Leica microtome (Leica Microsystems,Wetzlar,Germany) onto positively charged glass slides and stained with hematoxylin-eosin and examined under light microscopy.
All immunohistochemical assays were performed on the Ventana Discovery research platform (Ventana Medical Systems,Tucson,Arizona,USA).Biopsy materials were analyzed with immunohistochemistry for SARS-CoV-2 nucleocapsid protein and angiotensin-converting enzyme 2 (ACE2) receptor.
After antigenic retrieval,ACE2 receptor (Abcam,ab108252) and SARS-CoV-2 nucleocapsid protein (Abcam,ab273167) were used for all specimens with an optimized dilution of 1/200.Secondary labeling and staining were performed based on streptavidinbiotin horseradish peroxidase on the Omni-UltraMAP HRP(Ventana Medical Systems,Tucson,Arizona,USA) following the duration and protocols of the device and kit,then the samples were colored with diaminobenzidine and background stained with Mayer’s hematoxylin.Membranous staining with the ACE2 antibody,cytoplasmic,and/or nuclear staining for the SARS-CoV-2 nucleocapsid protein was considered positive.Staining percentages in the tissues were evaluated,and comparing the intensity was not used.Kidney tissue positive for ACE2 and lung tissue for nucleocapsid protein were used as positive controls.Phosphatebuffered saline was used instead of primary antibody for negative control.
2.3.3.Analysis of fungi and parasites in lung tissues
In the nine lung biopsy materials,the presence ofAspergillus fumigates(A.fumigates),Pneumocystis jirovecii(P.jirovecii),Microsporidia,Cryptosporidiumspp.,andToxoplasma gondii(T.gondii) were analyzed by using the RT-PCR tests after DNA isolation.
2.3.4.DNA isolation
For DNA isolation of the samples,25 mg of tissue samples were added into tubes with glass beads and centrifuged with Magna Lyser Rotor (Roche Diagnostics GmbH,Mannheim,Germany) at 5 000×rpm for one minute.Then,according to the manufacturer’s instructions,DNA was isolated using a tissue isolation kit (Qiagen GmbH,Hilden,Germany).The quantity and quality of DNA were assessed by the absorbance at A280/A260and A260/A230ratios using Nanodrop-ND1000 (Thermo Fisher Scientific,Waltham,Massachusetts,USA) and stored at -80 °C until the PCR test.
2.3.5.Real-time polymerase chain reaction
RT-PCR was performed on LightCycler®480 System (Roche Diagnostics GmbH,Mannheim,Germany).SYBR green,TaqMan,and hybridization master mixes were used for amplifications.Quantification was achieved using six serial 10-fold dilutions of the plasmids containing the target.We used internal and external controls for each sample[12-17].All PCRs were performed in triplicate.Primers,probes,target genes,and amplicon size are shown in Table 1.

Table 1.Primers and probes used in the diagnosis of microorganisms.
2.4.Variables
Demographic data (age,sex),body mass index,smoking history,symptoms on hospital admission,comorbidities,and previous medications were screened.All medications used for the treatment of COVID-19,antimicrobial therapies,convalescent plasma transfusions,corticosteroids,and immunomodulatory therapies were recorded.
All patients were screened for significant events and therapies,including vasopressor requirement,need for invasive mechanical ventilation (IMV),renal replacement therapy,acute kidney injury(AKI),deep venous thrombosis,pulmonary thromboembolism (PTE),ventilatory-associated pneumonia (VAP),acute respiratory distress syndrome (ARDS),cardiac injury,acute myocardial infarction,and cardiopulmonary resuscitation.The dates of first COVID-19 symptoms,RT-PCR test positivity,and hospital admissions were also recorded.
2.5.Other definitions
ARDS and AKI were diagnosed according to the Berlin definition[18]and Kidney Disease: Improving Global Outcomes criteria[19],respectively.Cardiac injury was identified if the serum concentration of high-sensitive troponin I level was above the upper reference limit (URL) (> 42.9 ng/L)[20].VAP was defined as changes in sputum characteristics such as an increase in the amount of tracheal secretion,increased purulence,darkening in color,and ≥ 105CFU/mL reproduction in an endotracheal aspiration sample 48 hours after intubation[21].According to a previous study,hepatic injury was defined and categorized into three groups.It was defined as mild if alanine transaminase (ALT) was higher than the URL but less than two times the URL,moderate if ALT was between two to five times the URL,and severe if ALT was greater than five times the URL[22].
2.6.Primary and secondary outcomes
The primary outcome of the study was to define histopathologic and immunohistochemical features of postmortem biopsy specimens obtained from the lungs,heart,liver,and kidneys in patients who died from COVID-19.The secondary outcomes were to reveal the presence of SARS-CoV-2 in all tissues,as well as the presence of fungi and parasites in lung tissues by using RT-PCR tests after DNA isolation.
2.7.Statistical analysis
Statistical analysis was conducted with SPSS 24.0 (Statistical Package for the Social Sciences Version 24.0;IBM Corporation,Armonk,New York,USA).Continuous variables were presented as median (Q1,Q3) or mean±standard deviation and categorical variables as counts and percentages.
3.Results
3.1.Patient characteristics
The mean age of the patients was (70±12) years old,and half of them were male.The data,including patients’ characteristics,symptoms on hospital admission,past medical and drug history,all therapies,significant events related to organ injuries and the length of duration from the first symptom,RT-PCR test positivity,and hospital admission to death,are presented in Table 2.In brief,the mean body mass index was (26.6±6.0) kg/m2,and the half of patients had a smoking history.The most common symptoms on hospital admission were dyspnoea (91.7%),cough (50.0%),and fever(25.0%).Hypertension (66.7%),diabetes mellitus (DM) (25.0%),and coronary artery disease (16.7%) were the most common comorbidities.Additionally,lung pathologies,asthma,chronic obstructive pulmonary disease,and lung cancer were present in one patient (8.3%) each,and one patient had a history of congestive heart failure (8.3%).Of them,one patient (8.3%) had hemodialysisdependent chronic kidney disease.The rate of the patients with no comorbidity was 25.0%.All patients received a protocol-based standard therapy,including favipiravir,corticosteroid,enoxaparin,acetylsalicylic acid,dipyridamole,and proton pump inhibitor.Of them,16.7% received immunomodulatory therapy containing tocilizumab or anakinra.ARDS and vasopressor requirements were seen in all patients.Other notable events were VAP (75.0%),cardiac injury (66.7%),AKI (66.7%),and hepatic injury (58.3%).In addition,the patients received a median dose of 12.2 (4.7,22.8) mg/kg corticosteroids,equivalent to methylprednisolone.The median duration lengths from the first symptom and hospital admission to death were 21 (12,27) days and 15 (8,23) days,respectively.
3.2.Laboratory findings
The worst laboratory data values during hospitalization are summarized in Table 3.Almost all patients had high levels of infectious markers,elevated inflammatory cell counts,and lymphopenia.The median hemoglobin value was 7.8 (7.4,9.0) g/dL.The median partial pressure of oxygen/fraction of inspired oxygen(PaO2/FiO2) ratio was 77.4 (61.3,91.7).The median renal function test results showed increased creatinine and blood urea nitrogen levels,as well as decreased estimated glomerular filtration rate compared to the baseline.Laboratory tests revealed increased median levels of cardiac markers and increased levels of liver markers.The highest median D-dimer level was 7.45 (4.00,18.32) μg/mL.
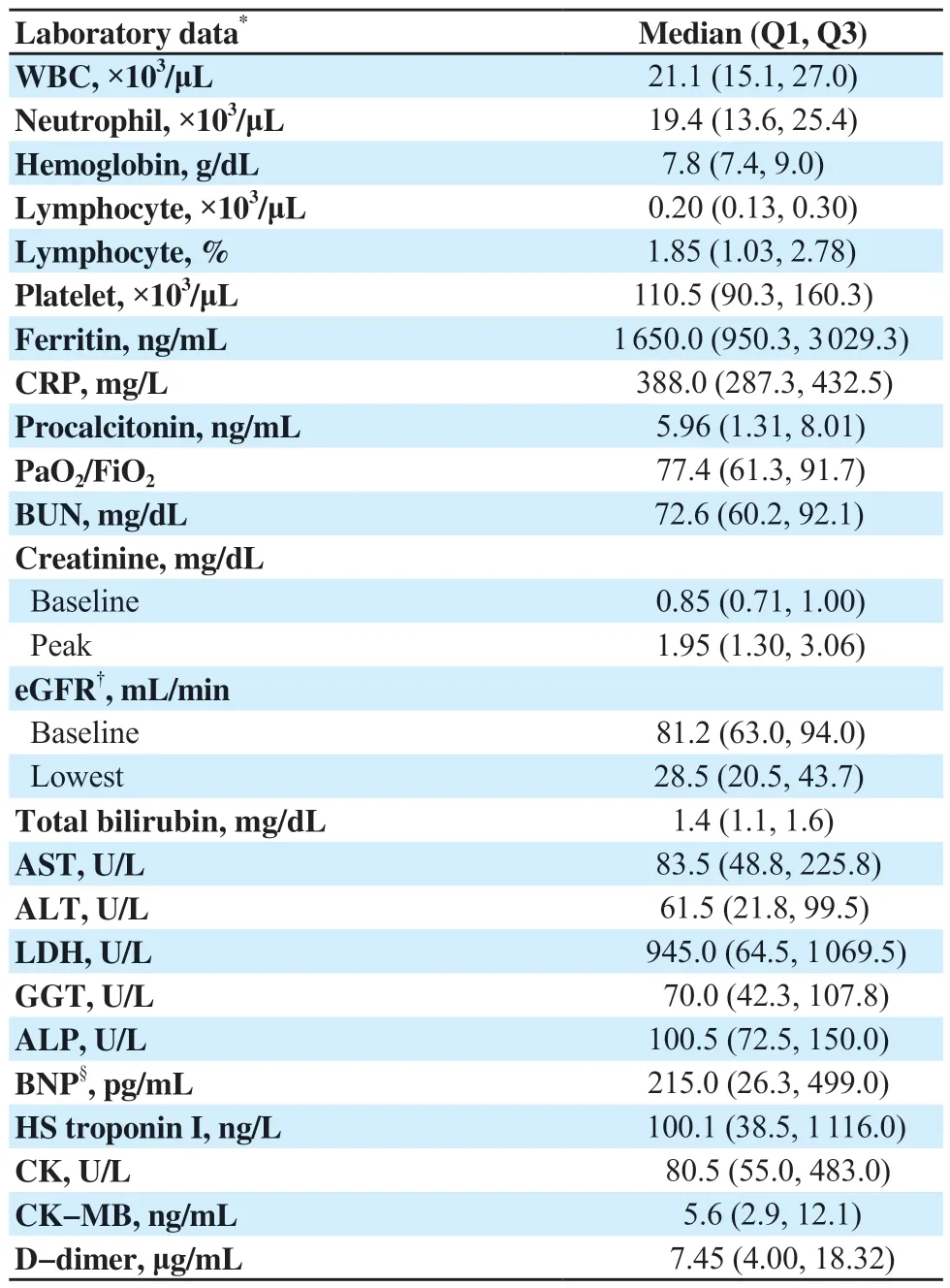
Table 3.Laboratory data of the patients (n=12,median,Q1,Q3).
3.3.Histopathologic findings
Of all,one heart and four lung biopsy specimens were not suitable for pathologic evaluation.Almost all patients had alveolar epithelial cell damage (87.5%).Diffuse alveolar damage (50%)(Supplementary Figure 1A and 1B),fibroblastic proliferation (50%),and fibrin deposition (75%) (Supplementary Figure 1C),and type II pneumocyte hyperplasia (50%) were other common findings.Hyaline membrane formation was only seen in one patient (12.5%).Also,patients had various patterns of inflammatory infiltration in the lungs.Heart biopsy specimens only indicated lymphocytic inflammatory infiltration in one patient (9.1%) (Supplementary Figure 1D).
Pigmented casts (58.3%),non-isometric vacuolar degeneration(41.7%),and capillary plugging (33.3%) (Supplementary Figure 1E) were frequently seen in the kidneys.Glomerulosclerosis and hemosiderin deposits were seen in two patients (16.7%).The pathological evaluation of kidneys revealed brush edge loss,necrosis,hemosiderin deposits,pigmented casts,interstitial inflammation,diffuse proximal tubule injury,and fibrosis in one patient with the comorbidity of hemodialysis-dependent chronic kidney disease,as expected.Additionally,interstitial inflammation,hemorrhage,and vasculitis were notable in one patient (8.3%).
Lobular lymphocyte infiltration (58.3%) and centrilobular sinusoidal dilatation (41.7%) were the most common findings in the liver specimens (Supplementary Figure 1F).On the other hand,spotty necrosis and fibrosis were remarkable findings in one patient (8.3%) (Supplementary Figure 1G).Also,fatty changes(Supplementary Figure 1F) were seen in the patients with various intensities.
3.4.Immunohistochemical findings and tissue SARS-CoV-2 RT-PCR test results
SARS-CoV-2 nucleocapsid protein antibody was detected in one lung and two kidney tissues of three patients (Supplementary Figure 1H,and 1I).In addition,SARS-CoV-2 nucleocapsid protein antibody was also found in distal tubular epithelial cells and glomerular capillary endotel in one patient (Supplementary Figure 1J).However,the RT-PCR test showed positivity in the lung tissues of three patients and the kidney tissues of two patients.ACE2 receptors in the lung tissue were only detected in one patient(12.5%) (Supplementary Figure 1K).Heart biopsy specimens indicated no immunohistochemical findings.ACE2 receptor positivity was detected in more than half of the patients in the kidney biopsy specimens (Supplementary Figure 1L).
3.5.Fungi and parasites in lung tissues
In biopsy samples,P.jiroveciiwas discovered in samples of all cases.In addition,Microsporidiain three (33.3%),A.fumigatusin two(22.2%),andCryptosporidiumspp.in two (22.2%) were detected.T.gondiiwas not found in any of the patient samples.
4.Discussion
In this study,we presented clinical and laboratory data of the patients who died due to COVID-19 and histopathological and immunohistochemical features in postmortem biopsy specimens sampled from the lungs,heart,liver,and kidneys.We also investigated the presence of SARS-CoV-2 in the tissues as well as the presence of fungi and parasites (P.jirovecii,Cryptosporidiumspp.,T.gondii,Microsporidia,andA.fumigatus) in lung tissues by RT-PCR test.Histopathological evaluation revealed different phases of ARDS in lung tissues,nonspecific changes in heart tissues,drug-related toxicity,and effects of cytokine storm triggered by SARS-CoV-2 in liver tissues,and findings related to rhabdomyolysis,myoglobinuria,and thrombotic microangiopathy in kidney tissues.ACE2 receptor and SARS-CoV-2 nucleocapsid protein antibodies were commonly shown in kidney and lung tissues,and SARS-CoV-2 RT-PCR tests were positive in liver,kidney,and lung tissues.
SARS-CoV-2 has a tropism to lung tissue and causes ARDS[23].In this study,different phases of ARDS with diffuse alveolar damage were the predominant pattern in the lung tissues.Smoking history,VAP,pulmonary comorbidities such as asthma,chronic obstructive pulmonary disease,and lung malignancy were the possible predisposing factors for lung damage.Additionally,all patients needed to have IMV.Mariniet al.[24]defined the COVID-19-associated ARDS (CARDS) types with different lung mechanics and clinical features.According to these definitions,an individualized mechanical ventilation strategy may contribute to the prevention of lung injury in patients with CARDS.However,the increased respiratory drive may cause lung injury by increasing the intensity of tidal strains and energy loading on vulnerable lung tissue in patients with excessive inspiratory efforts[25,26].Likewise,spontaneous pneumomediastinum and pneumothorax[27]occurred without positive pressure ventilation in the non-hospitalized patients demonstrating the importance of an individualized mechanical ventilation strategy.Corticosteroids,antiviral,and anti-cytokine therapies may decrease lung injury in patients with CARDS[2-4],but new studies are needed to prevent permanent damage patterns such as fibrosis by using anti-fibrotic therapies[28].
The rate of COVID-19-related cardiac injury is up to 50% in critically ill patients[29].The possible pathophysiological mechanisms are the direct effect of immune response on myocardium,stressinduced cardiomyopathy causing impaired oxygen delivery,and deterioration of ventricle functions due to ARDS,PTE,and positive pressure ventilation[9,30].In previous studies,myocarditis[9,31,32],myocyte necrosis[31],cardiomyopathy,interstitial edema[33],and microvascular arterial thrombosis[31]were the histopathological findings in patients with COVID-19-related cardiac injury.Despite the high rate of laboratory-diagnosed cardiac injury in this cohort,lymphocytic inflammatory infiltration was seen in only one patient which did not indicate myocarditis according to the Dallas criteria[34].As a result of this,cardiac events were transient in this cohort.
Possible mechanisms for COVID-19-related acute liver injury were defined as ACE2-mediated direct viral effects,cytokine storm,and drug-induced injury in the literature[14].Patients with severe liver injury (patients 3 and 12) in the present study have previously defined risk factors,including male sex,severe course of COVID-19,vasopressor requirement,and high procalcitonin levels indicating septicemia[16,35].Patient 3 also had metabolic factors such as DM,hypertension,and obesity[36].Severe hypoxemia and the need for positive pressure ventilation that caused increased right ventricular afterload might be the other predisposing factors in these patients.Although some studies have claimed otherwise[35],young age is related to severe liver injury in patients with COVID-19[16].Likewise,the patients diagnosed with severe acute liver injury were the youngest members of this cohort.
The use of multiple antimicrobial agents and steroids might be the underlying reason for drug-induced liver injury which was the predominant pattern in this cohort.However,cytokine storm triggered by SARS-CoV-2 might be a facilitating factor for these findings.Risk factors for hepatosteatosis (obesity,DM,and hypertension) were common in patients with microvesicular steatosis.Immunomodulatory therapies,including tocilizumab and anakinra,may cause a transient increase in ALT[37],but in this cohort,anakinra or tocilizumab administration did not cause an increase in liver enzymes.
AKI is an independent risk factor for mortality in patients with COVID-19 with rates of 64% in critically ill patients and 86.9%in invasively ventilated patients[38].Many interrelated factors may cause AKI in patients with COVID-19[6,7].The potential effects of SARS-CoV-2 and ACE2 interaction on the renin-angiotensinaldosterone system,direct cellular damage,humoral immune response,and cytokine storm are the possible mechanisms.Also,clinical conditions such as septicemia and ARDS,and prothrombotic nature of the disease caused impaired intrarenal microcirculation and decreased tissue oxygen delivery in these patients[5-7].In this cohort,ARDS,IMV requirement,vasopressor need,septicemia,and nephrotoxic drug exposure were the predisposing factors for AKI.
In this cohort,the pigmented cast was a frequent histopathological finding defined as an independent risk factor for the recovery from AKI in patients with COVID-19.It is also associated with nephrotoxic antibacterial medications and myoglobinuria secondary to rhabdomyolysis[5,7],but the laboratory data did not indicate rhabdomyolysis in any patient.However,colistin was frequently prescribed to patients with the pigmented cast.
SARS-CoV-2 induces hypercoagulation and thrombosis[39].In addition,septicemia,ARDS,and possible IMV-induced biotrauma were common in this cohort.Despite the use of an antiaggregant and anticoagulant combination,the high incidence of thrombotic microangiopathy and capillary plugging may be explained by the increased tendency to hypercoagulation during the disease course.Almost all patients had high D-dimer levels,but none were diagnosed with deep venous or PTE.
The most common glomerular pathology in recent studies in patients with COVID-19 is collapsing glomerulopathy[5,6,8].In the present study,no glomerular pathology was defined except one patient.Previous studies determined an association between the collapsing glomerulopathy and viral infections,including human immunodeficiency virus or Parvovirus B19 with the possible pathophysiological mechanisms of increased interferon production and cytokine-induced podocyte injury[5,6]in patients with apolipoprotein L1 high-risk alleles.Likewise,these mechanisms are possible for SARS-CoV-2,especially in African-American patients with apolipoprotein L1 high-risk alleles[40].In the present study,we did not perform any genetic analysis and all patients were Caucasian.
Although intracellular viral or spike protein-like particles were shown in previous studies,direct cellular infection of SARS-CoV-2 has not been based on clear evidence[5-7,41].However,viral RNA and SARS-CoV-2 transcripts were shown in two case reports[42,43].In this study,RT-PCR test,and SARS-CoV-2 nucleocapsid protein antibody positivity in the tissues might not be sufficient to present a piece of clear evidence for direct cellular infection due to the lack of ultrastructural findings.
Corticosteroids and cytokine blockers were used in patients with COVID-19 to prevent hyperimmune response and cytokine storm[3].However,opportunistic infection agents were detected in some of these patients[10].Although no patients had a history of humoral or cellular immunodeficiency in this cohort,P.jiroveciiwas detected in nine lung biopsies.The non-contrast enhanced thorax computed tomography on admission did not indicate any suspicious findings forP.jiroveciiin these patients.Biopsy sampling from these patients was carried out with a few months of variation.Also,the patients were hospitalized in different ICUs.Thus,an in-hospital epidemic ofP.jiroveciiwas not possible.However,due to the lack of suspicion,further diagnostic tests forP.jiroveciiwere not performed in these patients.
The risk factors of invasive pulmonary aspergillosis in patients with COVID-19 are presented in a previous study[44].Of patients with invasive pulmonary aspergillosis,the histopathological evaluation revealed destruction.Patients withA.fumigatusalso had corticosteroid and multiple antibiotics uses and conditions related to lung destruction.
Lung involvement ofMicrosporidiaandCryptosporidiumspp.in patients with COVID-19 has not been shown yet.The possible mechanism of respiratory transmission ofCryptosporidiumspp.remains unclear.Moret al.[45]defined the mechanism of respiratory transmission as inhaling oocysts.However,respiratory transmission is more likely forMicrosporidia[46].In previous case reports,lung involvement ofMicrosporidia[47]andCryptosporidiumspp.[48]were shown in patients with acquired immunodeficiency.In this cohort,decreased acid secretion from gastric mucosa due to the use of proton pump inhibitors,and sedation-suppressing oropharyngeal reflexes might be predisposing factors causing micro aspiration through the lungs of these agents.
The present study demonstrated many opportunistic infectious agents in the lungs.Lymphopenia,altered lymphocyte functions[49],and corticosteroid use[3]in patients with COVID-19 may cause an increased risk for lung involvement of fungal and parasitic microorganisms.In these cases,we recommend more frequent bronchoalveolar lavage sampling with the other diagnostic tests,even if there is no clinical,laboratory,or radiological suspicion.
The study is limited by its descriptive nature.Another limitation is the lack of further examinations,such as electron microscopic analysis.However,the study has some strengths.Compared to the autopsy series,sampling in the early postmortem period has revealed more reliable data.Immunohistochemical analysis and tissue RT-PCR test were performed to research the direct viral cellular infection.Also,multi-organ biopsy sampling for each patient,supporting the findings with clinical and laboratory data,contributed to defining the systemic infectious nature of SARS-CoV-2.Finally,many kinds of opportunistic microorganisms that have not been demonstrated yet in critically ill patients with COVID-19 were defined using RT-PCR tests after DNA isolation from the lung tissues.However,novel studies including larger sample sizes are needed to generalize the results.
In conclusion,COVID-19 is a multi-systemic disease that may cause lung,heart,liver,and kidney injury.Possible pathophysiological mechanisms include direct cytopathic effect,dysregulated immune response,and cytokine storm.Septicaemia,vasopressor requirement,hypoxemia,need for IMV,and thromboembolic events might exacerbate organ injury.A multidisciplined approach is essential to manage the disease with strategies for reducing organ injury.Additionally,corticosteroids and anti-cytokine therapies might predispose COVID-19 patients to opportunistic infections,though these therapies reduce mortality.
Conflict of interest statement
The authors report no conflict of interest.
Funding
Dokuz Eylül University Scientific Research Projects Coordination Unit funded the study (grant no.2020.KB.MLT.001).
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors'contributions
All authors contributed to the concept development,data analysis,manuscript preparation,editing,and review.MNY,ÖUB,FB,BE,BC,AC,SA,and ANG: design of the study.MNY,FB,ESU,BE,BC,AC,SA,and ANG: definition of intellectual content.MNY,BE,AE,ÖG,TÇA,ÖUB,SA,and ANG: literature search.MNY,BE,AE,ÖG,TÇA,ÖUB,AC,SA,and ANG: data acquisition.MNY:statistical analysis.
 Journal of Acute Disease2023年5期
Journal of Acute Disease2023年5期
- Journal of Acute Disease的其它文章
- Efficacy of Willis covered stent of intracranial pseudoaneurysms in the internal carotid artery: A systematic review and meta-analysis
- Intention and hesitancy to receive a booster dose of COVID-19 vaccine among pregnant women using a health belief model: A cross-sectional study
- Mechanical ventilation and outcomes in COVID-19 patients admitted to intensive care unit in a low-resources setting: A retrospective study
- Diagnostic value of ABCD2 and ABCD3-Ⅰ risk scoring systems in determining one-month risk of stroke in patients with transient ischemic attack: An observational study
- Cardiovascular sequelae in post-COVID-19 patients with moderate to severe CT severity score: A follow-up study
- Penetrating soft palate injury by lollypop candy stick
