Diagnostic value of ABCD2 and ABCD3-Ⅰ risk scoring systems in determining one-month risk of stroke in patients with transient ischemic attack: An observational study
Tuncay Aslan,Serkan Emre Eroğlu,Mehmet Muzaffer İslam,Serdar Özdemir,Gökhan Aksel,Abdullah Algın
Department of Emergency Medicine,University of Health Sciences Umraniye Training and Research Hospital,Istanbul,Turkey
ABSTRACT Objective: To compare the diagnostic value of the ABCD2 and ABCD3-Ⅰ scoring systems in predicting the development of a 30-day neurological event in adult patients with transient ischemic attack (TIA) presenting to the emergency department.Methods: The study was observational and prospective and was conducted in a single center.The diagnostic values of the ABCD2 and ABCD3-Ⅰscores in predicting a neurological event within one month were compared in patients diagnosed with TIA in the emergency department.Results: A statistically significant difference was observed between groups with or without stroke within one month in terms of both the ABCD2 and ABCD3-Ⅰscores (P=0.044 and P=0.029,respectively).There was no statistically significant difference between the patients with and without a recurrent TIA within one month in relation to the ABCD2 score (P=0.934),but a statistically significant difference was found in the ABCD3-Ⅰscores of these groups (P<0.001).Conclusions: Both the ABCD2 and ABCD3-Ⅰscoring systems could predict ischemic stroke within 30 days of TIA,the ABCD3-Ⅰscore is more effective than the ABCD2 score in the prediction of TIA recurrence.
KEYWORDS: Transient ischemic attack;Stroke;Emergency services;Risk reduction behavior;Risk assessment;Risk factors
1.Introduction
Stroke is a clinical condition that suddenly occurs for no apparent reason other than a vascular cause,leads to focal or global cerebral dysfunction,and lasts for 24 hours or longer or results in death.Globally,stroke ranks third among the causes of death after cardiovascular diseases and cancer[1,2].Since there are different views concerning whether patients with a transient ischemic attack(TIA) should be treated as an outpatient or hospitalized[2],the question of which patient may have a stroke within a short time of TIA has gained importance.To answer this question,some criteria are used to predict the clinical status of patients.
The most commonly used risk scoring systems for the prediction of stroke are ABCD2 and ABCD3-Ⅰ[3].In addition to the parameters of the ABCD2 scoring system,ABCD3-Ⅰincludes dual TIA (at least one more TIA that occurs within seven days of the first TIA and requires medical attention),carotid imaging findings (presence of ipsilateral ≥50% internal carotid stenosis),and presence of hyperintensity on acute diffusion-weighted imaging (DWI)[3].In addition,recently,scoring systems have been examined by determining various durations in terms of stroke risk after TIA.The current study aimed to compare the diagnostic value of the ABCD2 and ABCD3-Ⅰscoring systems in predicting the development of a 30-day neurological event in adult patients presenting to the emergency department with TIA.
2.Patients and methods
2.1.Study design and setting
This study was an observational,prospective,diagnostic,and predictive study and conducted in a single tertiary center between September 1,2020,and September 30,2021.Informed consent was obtained from all the patients included in this study.
2.2.Inclusion and exclusion criteria
The inclusion criteria were as follows: being aged 18 years or older,agreeing to participate in the study,and having neurovascular symptoms and a diagnosis of TIA confirmed by the neurologist consulted.Patients with incomplete data in their medical records(could not follow up) were excluded from the study.
2.3.Data collection
Airway,respiratory,and circulatory systems were evaluated upon arrival.Heart rate,systolic and diastolic blood pressures,and peripheral oxygen saturation were measured.In addition,patients’demographics characteristics and chronic diseases were recorded.Laboratory tests and imaging exams were performed for diagnosis and treatment.
For each patient,the ABCD2 and ABCD3-Ⅰscores and modified Rankin score (mRS) were calculated,and the results were recorded in the follow-up form.The outcomes (discharge,hospitalization,or withdrawal treatment),and 30-day follow-ups were also recorded.
2.4.Outcomes
The primary outcome was the diagnostic value of the ABCD2 and ABCD3-I scoring systems in predicting the development of a 30-day neurological event.Patients who had a repeat TIA or a new ischemic stroke within 30 days of the patient’s admission to the emergency department with TIA were defined as 30-day neurological events.The primary outcome of the study was composite.The secondary outcome was the comparison of the diagnostic performance of these two scoring systems in predicting the risk of stroke within six months and the risk of a recurrent TIA within 30 days,as well as the diagnostic value of mRS in predicting the risk of a neurological event within 30 days,scoring systems in predicting the development of a 30-day neurological event.Patients who had a repeat TIA or a new ischemic stroke within 30 days of the patient’s admission to the emergency department with TIA were defined as 30-day neurological events.
2.5.Statistical analysis
Categorical data were expressed as frequency and percentages.The distribution of continuous data was tested with the Shapiro-Wilk test.All continuous data showed a non-normal distribution and therefore were expressed as median (Q1,Q3).The Mann-Whitney U test was used for the pairwise group comparisons of continuous data.The receiver operating characteristics (ROC) test was used to calculate the diagnostic performance of the scoring systems,and the area under the curve (AUC) values were calculated.AUC values above 0.7 were accepted as statistically significant[4].The DeLong test was used to compare the AUC values[5].The value with the highest sum of the sensitivity and specificity of each scoring system was calculated with the Youden index.This value was accepted as the optimal cut-off value,and the diagnostic test performance criteria of the scoring were calculated according to this threshold.The statistically significant level was accepted asP<0.05.
2.6.Ethical statement
It was approved by the ethics committee (number: B.10.1TKH.4.34.H.GP.0.01/294,date: 13.08.2020).
3.Results
A total of 150 patients met the inclusion criteria,but 28 of these patients were excluded due to not follow up.A total of 122 patients were included (Figure 1).

Figure 1.The study flowchart.
3.1.Demographic and clinical characteristics
Of the 122 patients,57 (46.7%) were female,and the median age was 68 (55-77) years.Diabetes mellitus was present in 37 (30.3%)patients,hypertension in 65 (53.3%),and coronary artery disease in 15 (12.3%).Neurological symptoms were observed in 39 (32.0%)patients at the time of presentation.The median ABCD2 score was 4 (4-5),and the median ABCD3-Ⅰscore was 5 (4-7).Eighty-one(66.4%) patients were discharged from the emergency department after follow-up,31 (25.4%) were admitted to the inpatient wards,and 10 (8.2%) were recommended to be admitted to the inpatient wards but they did not accept this recommendation and left the hospital after signing the examination and treatment rejection form.TIA recurred within one month in 37 (30.3%) patients,and ischemic stroke developed within one month in 7 (5.7%) patients.The main descriptive characteristics of the patients are summarized in Table 1.

Table 1.Demographic and clinical characteristics (n=122).
3.2.Primary outcomes
As the primary outcome of the study,the diagnostic values of the ABCD2 and ABCD3-Ⅰscores in predicting ischemic stroke within one month of TIA were compared in patients diagnosed with TIA in the emergency department.The median ABCD2 score of the patients who had a stroke within one month of TIA was 5 (4-8),the median ABCD2 score of those who did not have a stroke within one month of TIA was 4 (4-5),and there was a statistically significant difference between the groups (P=0.044).When the diagnostic value of the ABCD2 score in predicting stroke within one month of TIA was examined with the ROC analysis,the AUC value was calculated as 0.720 [95% confidence interval (CI): 0.524,0.917](Table 2,Figure 1).

Table 2.Result of ROC analysis.
The median ABCD3-Ⅰscore was calculated as 8 (5-9) for the patients that had a stroke within one month of TIA and 5 (4-6) for those that did not have a stroke within one month of TIA,with a statistically significant difference (P=0.029).ROC analysis showed that the AUC value of the ABCD3-Ⅰscore was calculated as 0.743(95%CI: 0.540,0.946) (Table 2,Figure 2).There was no statistically significant difference between the AUC values of the ABCD2 and ABCD3-Ⅰscores in predicting the risk of ischemic stroke within one month of TIA (P=0.702,AUC difference:0.024,95%CI: -0.115,0.171,DeLong equality test).The optimal cut-off values of the ABCD2 and ABCD3-Ⅰscores in predicting stroke within one month of TIA were calculated as 6.5 and 7.5,respectively.
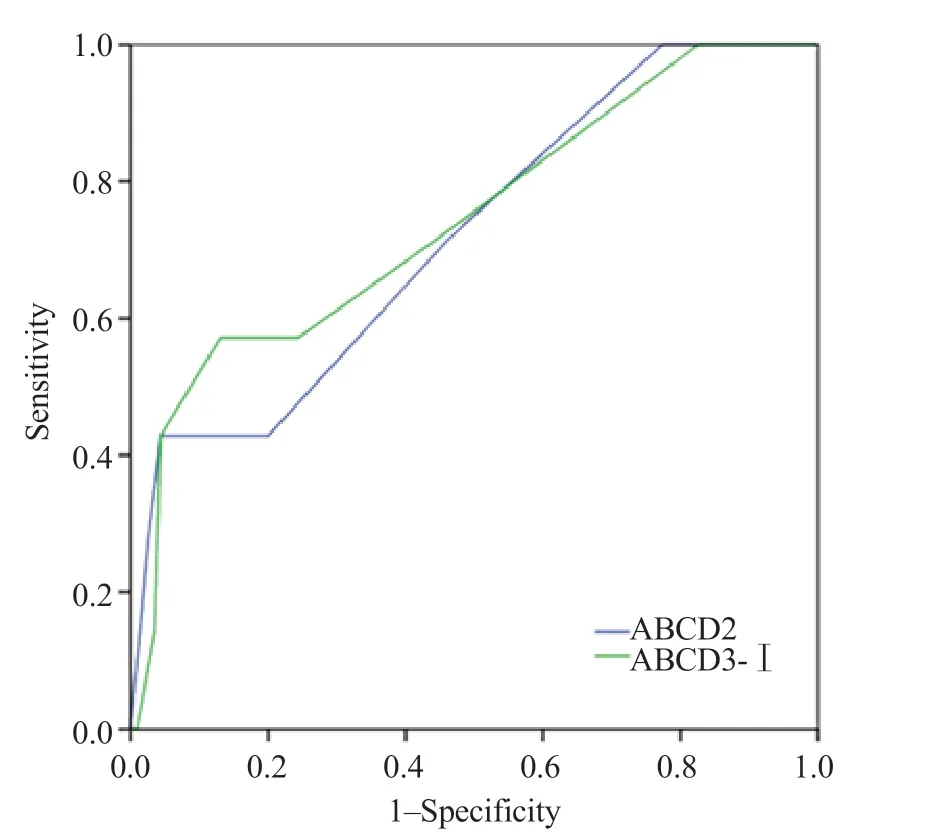
Figure 2.Receiver operating characteristic analysis for prediction of stroke within one month.
3.3.Secondary outcomes
As secondary outcomes,we examined the diagnostic value of the ABCD2 and ABCD3-Ⅰ scores in predicting ischemic stroke within six months of TIA and recurrent TIA within one month.
The median ABCD2 score of the patients who had an ischemic stroke within six months of TIA was 5 (4-8),the median ABCD2 score of those who did not have a stroke within six months of TIA was 4 (4-5),and the difference was not statistically significant(P=0.074).The median ABCD3-Ⅰscores of the patients who did and did not have an ischemic stroke within six months of TIA were 6 (5-9) and 5 (4-7),respectively,revealing no significant difference(P=0.105).
The median ABCD2 scores of the patients with and without a recurrent TIA within one month were both determined as 4 (4-5),with no statistically significant difference (P=0.934).The median ABCD3-Ⅰscores of the patients with and without a recurrent TIA within one month of the first TIA were 7 (6-8) and 5 (4-6),respectively,and the difference was statistically significant(P<0.001).
Patients with an mRS of 6 (indicating death) at the time of arrival at the emergency department were excluded from the study because they could not be followed up for one month.It was determined that the mRS values of all the patients who had a stroke within one month were ≥3.TIA recurred within one month in three (30%) of the 10 patients with an initial mRS of 0,11 (45.8%) of the 24 patients with an initial mRS of 2,18 (27.7%) of the 65 patients with an initial mRS of 3,four (19%) of the 21 patients with an initial mRS of 4,and one (50%) of the two patients with an initial mRS of 5 (Table 3).
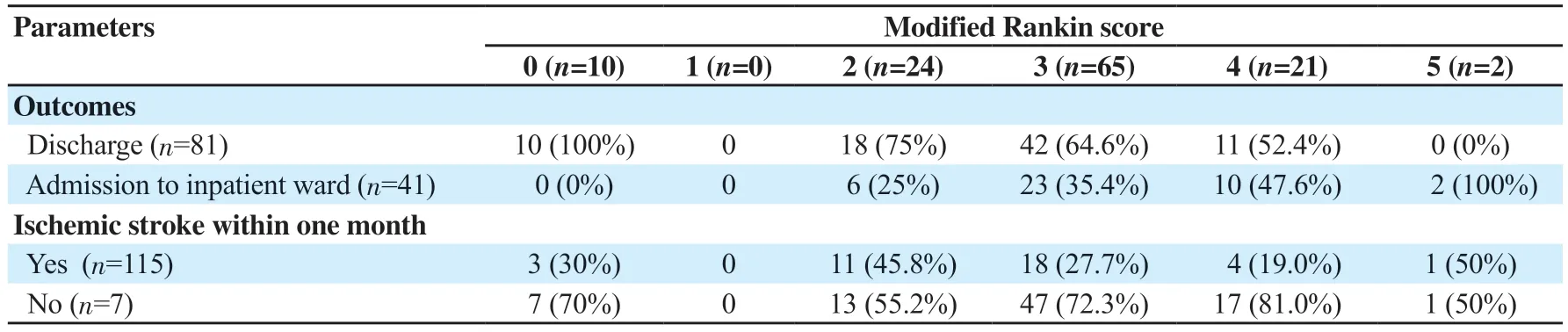
Table 3.Distribution of outcomes and occurrence of ischemic stroke within one month according to mRS values (n=122,n,%).
4.Discussion
In this study,we found that the ABCD2 and ABCD3-Ⅰscores could successfully predict the risk of stroke within one month of TIA.However,no statistically,significant difference was found in terms of the ability of the scoring systems to predict six-month stroke risk.In addition,there was no significant difference between the ABCD3-Ⅰand ABCD2 scores in terms of the prediction of a recurrent TIA within one month (P=0.702,DeLong equality test).
Stroke has serious consequences at individual,societal,and economic levels.It is among the leading causes of disability and loss of workforce and ranks third among the causes of mortality in Western countries and second in Turkey[1,6].Stroke patients constitute approximately half of all patients hospitalized due to neurological diseases,and the first evaluation of 2/3 of these cases is performed in emergency services[6].Therefore,the early recognition of patients with stroke risk in the emergency department can prevent comorbidities and mortality[7,8].
The ABCD and ABCD2 scoring systems were originally developed by primary care physicians and applied to triage patients at high stroke risk among those likely to be diagnosed with TIA.While some studies report that the ABCD2 score is useful in predicting stroke after TIA[9,10],others suggest that it is not useful for this prediction[11-14].This discrepancy may be because such studies are conducted with small populations in a single center,lack of diagnosis standardization of TIA (e.g.,general practitioners and neurology specialists),and evaluate different subgroups of TIA(definite or probable)[15,16].In a previous study,Fothergillet al.calculated the ABCD and ABCD2 scores of 284 patients with a preliminary diagnosis of TIA between 1985 and 1994 and evaluated the relationship between these scores and the outcome of stroke or death within the seven-day follow-up of the patients.The authors reported that although a score greater than 4 predicted stroke,some(25%) patients who developed stroke were in the low-or moderaterisk group according to these scoring systems[17].In another study conducted by Özpolatet al.,the ABCD2 risk scoring system was used to determine the risk of stroke within three days of TIA among patients who presented to the emergency department and reported a significant increase in the risk of stroke within three days of TIA in those with an ABCD2 score of 4 or higher[18].In the current study,we determined that an ABCD2 score greater than 5 predicted the development of stroke within one month of TIA.
In a prospective study,Engelteret al.reported that although the ABCD and ABCD2 scores could not predict some cases that developed stroke within 90 days,adding etiology and DWI findings to these scoring systems would be more useful in detecting those who might develop stroke.The authors found a higher rate of large artery arteriosclerosis and abnormal DWI findings in the etiology of stroke[19].In a prospective study,Songet al.developed a new scoring system (ABCD3-Ⅰ) by adding dual TIA,carotid artery,and DWI imaging findings to the ABCD2 score and evaluated the ability of this scoring system to predict a stroke within 90 days following TIA.They found that the ABCD3-Ⅰscore was superior to the ABCD2 score in predicting the development of stroke within 90 days of TIA[20].In a validation study performed by Takuyaet al.using the ABCD2,ABCD3,and ABCD3-Ⅰscoring systems,the incidences of stroke within 90 days and three years after TIA were found to be significantly higher in the high-risk group than in the low-risk group according to the ABCD2 score.When the same evaluation was made based on the ABCD3 score,it was found to be significantly higher in the intermediate-and high-risk groups than in the low-risk group for the three years after TIA.Lastly,according to the ABCD3-Ⅰscore,stroke risk was found to be higher in the high-risk group than in the low-and intermediate-risk groups[21].In our study,both the ABCD2 and ABCD3-Ⅰscores were found to be statistically significant (P=0.044 andP=0.029,respectively) in predicting a stroke within 30 days of TIA among the patients who presented to the emergency department with TIA.
In this study,the ABCD2 and ABCD3-Ⅰscores did not statistically significantly differ between the patients who did and did not develop an ischemic stroke within six months of TIA.And all the patients who had a stroke within one month after TIA had an mRS of ≥3.It is suggested that mRS calculation can be used in the prediction of stroke after TIA as an easy and cost-effective method since it does not require any additional examination.
Due to the single-center design of our study,sufficient population diversity may not have been achieved.In addition,we consider that the alleviation of patients’ complaints due to the nature of the TIA disease may have reduced their visits to the hospital.Furthermore,the COVID-19 pandemic during the study period led to a decrease in the number of patient presentations to the emergency department,which may have affected the sample size of our study[22].
In conclusion,ABCD2 and ABCD3-Ⅰscoring systems could predict the risk of a stroke within one month of TIA,but they could not predict the risk of stroke within six months of TIA.In addition,the ABCD3-Ⅰscore could successfully predict the risk of a recurrent TIA within one month,while the ABCD2 score does not have this predictive ability.Lastly,it is determined that the mRS values of all the patients with a stroke within one month of TIA are≥3.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors’ contributions
TA,SEE,MMİ,SÖ,and GA gave substantial contributions to the conception or the design of the manuscript;TA,SEE,SÖ,GA,and AA contributed to acquisition,analysis,and interpretation of the data.All authors have participated to drafting the manuscript.SÖ and SEE revised it critically.All authors read and approved the final version of the manuscript.All authors contributed equally to the manuscript and read and approved the final version of the manuscript.
 Journal of Acute Disease2023年5期
Journal of Acute Disease2023年5期
- Journal of Acute Disease的其它文章
- Efficacy of Willis covered stent of intracranial pseudoaneurysms in the internal carotid artery: A systematic review and meta-analysis
- Intention and hesitancy to receive a booster dose of COVID-19 vaccine among pregnant women using a health belief model: A cross-sectional study
- Mechanical ventilation and outcomes in COVID-19 patients admitted to intensive care unit in a low-resources setting: A retrospective study
- Cardiovascular sequelae in post-COVID-19 patients with moderate to severe CT severity score: A follow-up study
- Pathological and immunohistochemical findings of lungs,heart,liver,and kidneys,and unexpected findings of fungi and parasites in lungs of deceased COVID-19 patients: A case series
- Penetrating soft palate injury by lollypop candy stick
