Mechanical ventilation and outcomes in COVID-19 patients admitted to intensive care unit in a low-resources setting: A retrospective study
Sarakawabalo Assenouwe ,Tabana Essohanam Mouzou ,Ernest Ahounou ,Lidaw Déassoua Bawe ,Awèréou Kotosso ,Koffi Atsu AziagbeEyram Makafui Yoan Amekoudi,Mamoudou OmourouChimene Etonga Anoudem,Komi Séraphin Adjoh
1National COVID-19 Referral Hospital,Regional Hospital of Lomé Commune,Lomé,Togo
2Faculty of Health Sciences,University of Kara,Kara,Togo
3Faculty of Health Sciences,University of Abomey-Calavi,Cotonou,Bénin
4Faculty of Medicine,University of Ottawa,Ottawa,Canada
ABSTRACT Objective: To describe the strategies and outcomes of mechanical ventilation in a poorly equipped facility.Methods: This retrospective descriptive study included patients with COVID-19 who were admitted to the intensive care unit (ICU) and mechanically ventilated between September 1,2020,and May 31,2021.Data were collected from medical records and databases.Results: 54 Patients aged (62.9±13.3) years were included.Among these cases,79.6% had at least one comorbidity.On admission,all patients had hypoxia.The median peripheral oxygen saturation in room air was 76% (61%,83%).Non-invasive ventilation (NIV)was performed in 75.9% of the patients,and invasive mechanical ventilation (IMV) in 68.5%.IMV was performed on patients due to severe coma (8.1%),failure of standard oxygen therapy (27.0%),and failure of NIV (64.9%).An arterial blood gas test was performed in 14.8% of the patients.NIV failed in 90.2% of cases and succeeded in 9.8%.IMV was successful in 5.4% of cases,vs. 94.6% of mortality.The overall mortality rate of patients on ventilation in the ICU was 88.9%.The causes of death included severe respiratory distress syndrome (85.2%),multiple organ failure (14.8%),and pulmonary embolism (13.0%).Conclusions: The ventilation management of COVID-19 patients in the ICU with NIV and IMV in a scarce resource setting is associated with a high mortality rate.Shortcomings are identified in ventilation strategies,protocols,and monitoring.Required improvements were also proposed.
KEYWORDS: Coronavirus disease 2019;Intensive care unit;Hypoxia;Invasive ventilation;Non-invasive ventilation;Arterial blood gas
1.Introduction
COVID-19 is frequently responsible for respiratory impairment resulting in acute respiratory failure in severe and critical presentations[1,2].Thus,13%-36% of patients hospitalized with COVID-19 require admission to a high-dependency unit,or intensive care unit (ICU)[3,4].The management of COVID-19 patients often requires respiratory support,including mechanical ventilation.This management has faced several challenges such as bed saturation due to patient overflow,and shortages of equipment,drugs,consumables,and qualified personnel[5,6].Moreover,in low-resource countries such as ours,critical care units are scarce and sparsely equipped.Therefore,patient management,especially mechanical ventilation and its outcomes,differs from those reported in developed countries.Few studies have reported the experience of ICUs during the COVID-19 pandemic outbreak in Sub-Saharan Africa[7,8].In view of experience sharing,this study aims to describe mechanical ventilation strategies and outcomes in severely ill COVID-19 patients in a scarce resources setting.
2.Patients and methods
2.1.Study design and setting
We conducted a retrospective descriptive study for nine months,from September 1,2020,to May 31,2021,at the Regional Hospital of Lomé Commune.This was the National COVID-19 Referral Hospital,dedicated to the management of COVID-19 patients.As of May 2020,an ICU has been fitted out and equipped,becoming fully operational in late August 2020.The study period extended from the setting up of the ICU until the end of the first COVID-19 wave,which occurred from January to May 2021 in Togo[9].
The diagnosis of COVID-19 was based on laboratory identification of the severe acute respiratory syndrome coronavirus 2 through reverse transcription polymerase chain reaction with nasopharyngeal or oropharyngeal swabs.According to the World Health Organization’s definition of clinical syndromes associated with COVID-19,patients were categorized as mild,moderate,severe,and critical[10].Patients with severe and critical conditions were admitted to the ICU.Due to the unavailability of a high-dependency unit,some patients with moderate conditions who required more than 6 L/min oxygen flow,or continuous monitoring,were admitted to the ICU.
2.2.Ethical approval
This study was approved by the ethical committee and authorized by the hospital director.The patient’s consent was not required,since the research was designed retrospectively and only the records of the patients were studied.Data were collected in compliance with ethical standards.
2.3.Inclusion criteria
We included patients who were admitted to the ICU during the study period with a COVID-19 diagnosis and were placed on either IMV or NIV.Those with missing key data,such as ventilation mode,peripheral oxygen saturation (SpO2),or follow-up information,were excluded from analysis.
2.4.Data collection
Data were collected retrospectively from medical records,laboratory results,and imaging results including demographic data,comorbidities,clinical characteristics upon initiation of ventilation such as respiratory rate,SpO2,vital distress,and clinical severity category.Reasons for ventilation,ventilation modes,and parameters including tidal volume,fraction of inspired oxygen (FiO2),positive end-expiratory pressure (PEEP),and ventilation pressure were also recorded.Follow-up data on ventilatione.g.the best daily values of respiratory parameters and arterial blood gas were collected as well.
2.5.Ventilation outcomes
Ventilation success was defined as improvement or resolution of respiratory distress,with SpO2> 94%,resulting in weaning off the ventilator and back up to standard oxygen therapy or room air breathing.
NIV failure was defined as the non-improvement or worsening of respiratory distress with persistent hypoxia (SpO2< 90%) after one hour or the occurrence of other distress,requiring IMV or resulting in death.
IMV failure was defined as worsening respiratory distress with persistent hypoxia or the occurrence of other distress leading to death.
2.6.Statistical analysis
Data were extracted and analyzed using Epi Info 7.3.2 software(Epi Info™,Center for Disease Control and Prevention,USA).Qualitative variables were presented as mean±standard deviation,median,and interquartile range,while quantitative variables were expressed as frequency and percentage.
3.Results
During the study period,1 073 patients were admitted to the Regional Hospital of Lomé Commune,out of whom 171(15.9%) were in the ICU.Of these,61 patients (35.7%) received mechanical ventilation and were selected for the study.Upon further investigation,7 cases were excluded due to incomplete data.Thus,the remaining 54 patients were included for analysis (Figure 1).
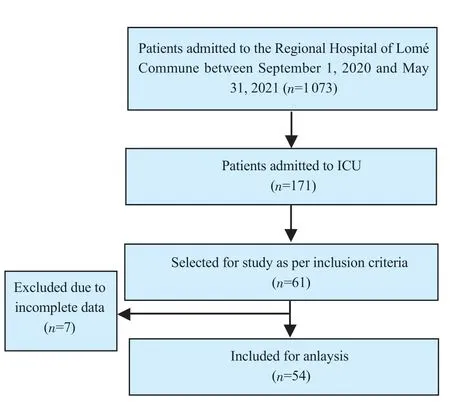
Figure 1.The study flowchart.
The mean age of the studied patients was (62.9±13.3) years ranging from 28 to 85 years,and the sex ratio was 1.1.Among the 54 patients,43 (79.6%) had at least one comorbidity,of which hypertension and diabetes were the most frequent,accounting for 61.1% and 44.4%,respectively (Table 1).

Table 1.Comorbidities,clinical features,and mortality risks of ventilated COVID-19 patients (n=54).
On admission to the ICU,all patients had dyspnea and hypoxia.The median SpO2on room air was 76% (61%,83%),and ranged from 15% to 91%.Out of all the patients,48 (88.9%) experienced respiratory struggle or exhaustion (Table 1).
A chest computed tomography scan was performed in 34 patients(63.0%).Ground glass opacity was found in 28 patients (51.9%),pulmonary embolism in 7 patients (13.0%),and crazy-paving pattern with pleural effusion in 4 patients (5.1%).Arterial blood gas was checked in 8 patients (14.8%),showing severe acute respiratory distress syndrome (ARDS) with a partial pressure of oxygen/fraction of inspired oxygen ratio(PaO2/FiO2)< 100 mmHg in 7 patients,and moderate ARDS (PaO2/FiO2ratio between 100 mmHg and 200 mmHg) in 1patient.The median PaO2/FiO2ratio,partial pressure of carbon dioxide,and pH were 133 (60,210) mmHg,51 (40,66) mmHg,and 7.36 (7.31,7.39),respectively.Among the 54 patients,52 (94.4%) received standard mask oxygen therapy before mechanical ventilation,and 2 (5.6%) were directly ventilated on admission.In addition,41 patients (75.9%) received NIV and 37 patients (68.5%) received IMV,corresponding to 44.0%and 35.0% of ICU patients,respectively.
NIV was initiated after the failure of standard oxygen therapy.Pressure-support ventilation with PEEP mode was used in 30 patients (55.6%),and continuous positive airway pressure mode in 24 patients (44.4%).The median SpO2was 88% (82%,92%) before NIV,and 89 (85%,91%) during NIV.
IMV was administered to 3 patients in comas (8.1%),10 patients of failure of standard oxygen therapy (27.0%),and 24 patients of failure of NIV (64.9%).Volume-assisted and controlled ventilation,pressure-assisted and controlled ventilation,and volume-controlled ventilation modes were applied in 34 (63.0%),25 (46.3%),and 22 patients (40.7%),respectively.The median SpO2was 85% (80%,90%) prior to IMV,and 88% (85%,92%) on IMV.Ventilation parameters are shown in Table 2.Medications or treatments given to ventilated COVID-19 patients including antithrombotic medications,antibiotic therapy,and antipyretics are listed in Table 3.

Table 2.Ventilation parameters in COVID-19 patients admitted to the intensive care unit (n=54).

Table 3.Treatments of ventilated COVID-19 patients in the intensive care unit (n=54).
NIV succeeded in 4 patients (9.8%),and failed in 37 patients(90.2%).Out of the 41 patients who received NIV,24 patients(58.5%) were switched to IMV,and 13 (31.7%) died on NIV.IMV was successful in 2 patients (5.4%),and the remaining 35 patients(94.6%) died.The overall mortality rate of patients on ventilation was 88.9%.The median length of stay in ICU was 7 (4,11) days ranging from 4 to 23 days.The common mortality factors were suspected or confirmed severe ARDS,pulmonary embolism,and multiorgan failure (Table 1).
4.Discussion
In this single-center retrospective study,both NIV and IMV were applied in the ICU.Patients were elderly and had comorbidities in most cases.NIV was associated with a high failure rate,requiring IMV or leading to death.
The high prevalence of comorbidities reported in our study has also been reported in the literature[1,11,12].Hypertension and diabetes were the most common comorbidities.Studies have shown that comorbidities,as well as advanced age,were associated with a high risk for severe COVID-19 patterns[13-15].Over half of the patients in our study were critical cases.However,due to the low rate of arterial blood gas tests,the management strategies were organized with a model of escalation based on clinical features: the patients received first conventional oxygen therapy unless they presented with severe coma or respiratory struggle or exhaustion.NIV was applied when oxygen therapy failed.Further,IMV was administered as the last option,in case of NIV failure,or severe respiratory distress with exhaustion or severe coma.In our cohort,the frequency of ventilation was low as well as in other low-income countries,where 4% to 26.2% of ICU patients received NIV and 2.5% to 28.7% received IMV[7,11,16].Unlike these findings,mechanical ventilation was widely used in middle-and high-income countries,with frequencies up to 92.8%[12,17,18].The low frequency of mechanical ventilation in our setting was related to the insufficiency of ICU ventilators,qualified critical care personnel,resuscitation consumables,and drugs,especially at the early stage of the pandemic.The COVID-19 pandemic outbreak has resulted in a major burden on ICU care,especially the availability of ventilators.NIV was the most-used respiratory support in our study.It has been used in other countries during the first waves of the pandemic,mainly because of the rapid increase in the number of severely and critically ill patients exceeding the capacity of the ICUs.As NIV could be performed outside the ICU,it has been an alternative to IMV,but with strict monitoring requirements.
In our setting,qualified critical care staff and sedation drugs were often insufficient to allow long-term sedation and IMV in conscious patients.Hence,NIV was used more than IMV.Early cohort studies appeared to establish that NIV was effective and could prevent intubation in patients with COVID-19-related ARDS[17,19].In contrast,randomized and multicenter cohort studies have not confirmed the effectiveness of NIV over high-flow nasal oxygen therapy in this condition[20,21].Therefore,NIV is no longer recommended as a first-line ventilator support method in COVID-19-related respiratory failure[22,23].Deaths on NIV might be attributed to inadequate indication for NIV,insufficient support of IMV,deficient monitoring,and the lack of resources to initiate IMV.This hypothesis was supported by the short ICU length of stay.High mortality rates under NIV were reported in the literature.Martiet al.found respectively 60.8% and 46.8% of failure and mortality rates on NIV[20].In a scarce resource setting during a humanitarian mission of Médecins Sans Frontières in Iraq,Thomaset al.reported a mortality rate of 61.1% on NIV[24].
High levels of PEEP were used in our study,as recommended in ARDS patients.However,ventilation pressures and volumes were higher than those recommended[25,26].Protective ventilation strategies are recommended for the management of ARDS in COVID-19 patients[22,25-28].High PEEP,low tidal volume,and low driving pressure were found to be effective in reducing mortality rates.
Ventilation monitoring was inadequate in our study.Arterial blood gas was infrequently reassessed,although this test was crucial in any respiratory distress.It was unavailable in our hospital at the beginning of the pandemic.Subsequently,shortages of consumables were noticed.Our study revealed other insufficiencies in ventilation strategies,such as the non-application of prone ventilation due to the lack of protective pads,and the unavailability of extracorporeal membrane oxygenation (ECMO) procedure.Prone ventilation and ECMO are additional strategies used in critically ill patients with ARDS,refractory to conventional ventilation[18,29,30].
The mortality rate reported in our study was high,as compared to studies in advanced intensive care facilities,where it ranged from 15% to 65% on mechanical ventilation[12,15,18,31,32].This high mortality rate of our cohort,even with IMV,could be attributed to late intubation with delayed IMV,and inadequate strategies of IMV.This has been confirmed by Nairet al.who reported significantly higher mortality in patients who were intubated later than those having early intubation and IMV (93.02%vs.66.66%)[13].
These discrepancies found in our setting suggest the need to improve ICU management of COVID-19 patients through the following recommendations: (1) train a sufficient number of skilled critical care staff,(2) enhance intensive care equipment,including high-flow nasal oxygen therapy,and ECMO,(3) increase supply of intensive care drugs,and consumables,and (4) upgrade intensive care protocols and monitoring.Ventilation protocols should be carried out in a stepwise treatment strategy while avoiding delayed intubation and invasive ventilation.
The limitation of the study included that the retrospective data collection method resulted in limited data availability,for example,not all ventilated patients were included in the analysis.The association of ventilation outcome with different parameters was also not assessed.Therefore,the determinant factors of the outcomes were not identified.Large cohorts and analytical studies could be conducted in the future to determine the potential factors associated with the outcomes.
Severe and critical COVID-19 patients admitted to the ICU were elderly and had comorbidities.They were managed for lifethreatening conditions,with respiratory distress being the most common.Respiratory support uses both non-invasive and invasive ventilation.Both methods were associated with high failure and mortality rates.Mortality was mainly due to infectious and respiratory complications.Shortcomings in ventilation strategies,protocols,and monitoring have been identified and require improvement.Our study has provided insight into the particular aspects of ventilator support for COVID-19 patients in scarce resource settings.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Acknowledgment
The authors would like to thank Doctor Lieutenant-Colonel Macamanzi A.Laroutoki,Director of the Regional Hospital of Lomé Commune,for authorizing and facilitating the study.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors'contributions
SA,TEM,EA,LDB,MO,and KSA: concept and design of the study.SA,TEM,EA,MO,and LDB: acquisition of data.SA,TEM,EA,AK,KAA,EYMA,MO,and CAE: analysis and interpretation of data.SA,TEM,EA,LDB,and AK: drafting the manuscript.KAA,MO,EYMA,CAE,and KSA: revising the manuscript.All authors gave final approval of the article.
 Journal of Acute Disease2023年5期
Journal of Acute Disease2023年5期
- Journal of Acute Disease的其它文章
- Efficacy of Willis covered stent of intracranial pseudoaneurysms in the internal carotid artery: A systematic review and meta-analysis
- Intention and hesitancy to receive a booster dose of COVID-19 vaccine among pregnant women using a health belief model: A cross-sectional study
- Diagnostic value of ABCD2 and ABCD3-Ⅰ risk scoring systems in determining one-month risk of stroke in patients with transient ischemic attack: An observational study
- Cardiovascular sequelae in post-COVID-19 patients with moderate to severe CT severity score: A follow-up study
- Pathological and immunohistochemical findings of lungs,heart,liver,and kidneys,and unexpected findings of fungi and parasites in lungs of deceased COVID-19 patients: A case series
- Penetrating soft palate injury by lollypop candy stick
